LDL-Cholesterol, or normally just referred to LDL, transfers fats around the body and supports immune function. However, too much LDL can block blood flow in the arteries and cause heart disease. Continue reading to learn about healthy LDL levels and how to lower LDL without medication.
What is LDL-Cholesterol?
Cholesterol is a fat-like substance that’s a key component of cells. It’s also used by the body to make steroid hormones (testosterone, estrogens, cortisol, aldosterone etc.), bile, and vitamin D [1].
Cholesterol that’s found in the blood is bound into particles called lipoproteins. You can think of lipoproteins as the vehicles and cholesterol as the passenger. These lipoproteins differ in density (vehicle size):
- LDL-cholesterol or low-density lipoprotein cholesterol is known as the “bad” cholesterol
- HDL-cholesterol or high-density lipoprotein cholesterol is known as the “good” cholesterol
- VLDL-cholesterol or very-low-density lipoprotein cholesterol is also a “bad” cholesterol
LDL-C forms in the blood when very low-density lipoprotein (VLDL) loses some fat (triglycerides) and becomes denser. It’s removed by the liver [2].
LDL- cholesterol is considered the “bad cholesterol” because it deposits in blood vessels. Cholesterol can penetrate arterial walls where it combines with oxygen (oxidizes). This is a key step in the development of hardening of the arteries and heart disease [3, 2].
LDL-C Components
LDL carries the most cholesterol of all lipoproteins. It is the major cholesterol carrier in the body. LDL contains [4]:
- Cholesterol
- Fats (triglycerides and other fats)
- Protein (Apoprotein B-100)
Functions of LDL
- Transfers fat and cholesterol around the body for cells to use [2].
- Binds certain toxins, making them unable to trigger harmful immune responses. LDL binds toxins produced by bacteria (Staphylococcus) and the toxin lipopolysaccharide (LPS) [5, 6].
- Helps repair damaged blood vessels. When arteries become damaged, LDL binds to the artery wall to aid the healing process. This helps the artery in the short-term but can be harmful long-term [7].
Oxidized LDL
When LDL gets inside the damaged artery wall to help the healing process, it undergoes a change and becomes oxidized. Oxidized LDL is toxic to artery wall cells. To remove oxidized LDL, inflammatory cells migrate to the artery wall [7].
Cholesterol, other fats, and more inflammatory cells can accumulate to form a fatty plaque in the artery. The plaque may grow large enough to restrict blood flow. For this reason, oxidized LDL contributes to heart disease [8].
In a meta-analysis (of 12 studies), those with oxidized LDL had a higher risk of heart disease [9].
LDL Types
LDL particles differ in size and density. Small, dense LDL particles are associated with higher heart disease risk than large, less dense particles. This is because small, dense LDL passes more easily into blood vessels and becomes oxidized [10].
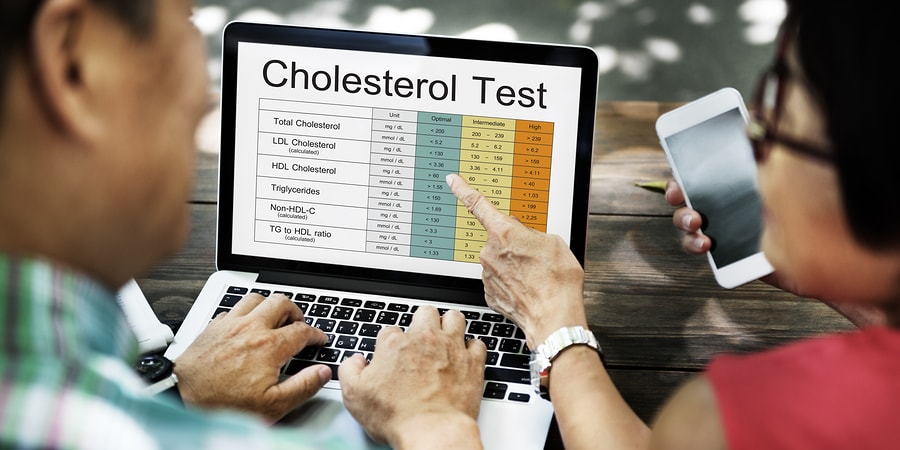
LDL-C Testing
A fasting LDL-C blood test estimates the amount of cholesterol carried by LDL particles. The following equation estimates LDL:
LDL-cholesterol = Total cholesterol – HDL-cholesterol – (Triglycerides/5) [11].
This equation can underestimate LDL-C if fat (triglycerides) levels are extremely high (> 400 mg/dL) [11].
LDL particles can also be directly measured in the blood, which is more accurate than the equation. However, this method is more expensive and not widely available [12].
The main factors affecting blood LDL-C levels are the amount of cholesterol that is [13]:
- Absorbed in the gut from food and bile
- Produced in the liver
- Used by cells
- Removed by the liver and HDL
The first two raise blood LDL, while the second two lower it.
Experts recommend that you check your cholesterol regularly, about every 5 years, or more often if you have a higher risk of heart disease, due to factors such as [14]:
- A family history of heart disease
- Smoking
- Being overweight/obese
- Having diabetes or high blood pressure
Optimal, Normal, and Elevated LDL-C Levels
Based on the National Cholesterol Education Program (NCEP), LDL-cholesterol levels are classified as:
- Optimal: < 100 mg/dL (2.59 mmol/L)
- Near optimal: 100-129 mg/dL (2.59-3.37 mmol/L)
- Borderline high: 130-159 mg/dL (3.37-4.12 mmol/L)
- High: 160-189 mg/dL (4.15-4.90 mmol/L)
- Very high: > 189 mg/dL (4.90 mmol/L)
If your levels are elevated, work with your doctor to set desired goals for LDL-C levels based on your individual risk factors. Elevated LDL-C can be addressed with dietary and lifestyle changes. In addition, your doctor may prescribe cholesterol-lowering drugs, such as statins, for certain high risk combinations of cholesterol levels and other heart disease risks.
Target values based on risk factors are usually:
- LDL-C < 100 mg/dL (2.59 mmol/L) for those with heart disease or diabetes
- LDL-C < 130 mg/dL (3.37 mmol/L) for those with 2 or more risk factors (intermediate risk for heart disease)
- LDL-C < 160 mg/dL (4.14 mmol/L) for those with 0 or 1 risk factors (low risk for heart disease)
Some recommend that LDL-C should be < 70 mg/dL (1.82 mmol/L) for those with heart disease [15].
LDL vs. HDL
LDL and HDL work together to maintain cholesterol levels. LDL delivers cholesterol from the liver to organs that use it. HDL gathers unused cholesterol from organs and returns it to the liver for reuse [16].
This table shows important differences between LDL and HDL [17, 18]:
High LDL-Cholesterol Levels
Causes
Causes listed below are commonly associated with high LDL-cholesterol. Work with your doctor or another health care professional to get an accurate diagnosis. Your doctor will interpret your results, taking into account your medical history, symptoms, and other test results.
1) Diets High in Calories and Saturated/Trans Fats
Many studies have shown that trans fats increase LDL-C [19, 20, 21, 22].
A similar relationship exists between saturated fat intake and LDL-C. In a meta-analysis of 60 studies, replacing carbs with saturated fat increased LDL-C [23].
Consuming a high-saturated fat diet for 3 weeks increased LDL-C and harmful (small, dense) LDL particles in a study of 53 adults [24].
Some people also experience larger LDL-C increases after high cholesterol meals or diets. Those people tend to absorb more cholesterol from their diet due to genetic differences [25, 26].
2) Physical Inactivity
In a study of 1,331 adults, physical inactivity was linked to higher LDL-C [27].
Low levels of physical activity and screen time (TV and computer games use) were also associated with higher LDL-C in studies of 574 youth [28, 29].
3) Obesity
In obesity, the number of harmful (small, dense) LDL particles increases. Total LDL-C levels increase slightly [30].
Obesity also reduces the number of LDL receptors in the body, which reduces response to LDL-C and raises its levels in the blood [31].
4) Hypothyroidism
A low-functioning thyroid gland (hypothyroidism) can increase LDL [32, 33].
In a study of 106 adults, patients with subclinical hypothyroidism had higher LDL than those with a healthy thyroid [34].
5) Insulin Resistance and Type 2 Diabetes
Patients with type 2 diabetes have elevated small, dense LDL particles and oxidized LDL. Total LDL-C levels remain normal or increase only slightly [35].
LDL particles remain in the blood longer for individuals with type 2 diabetes. This increases the likelihood of LDL-C depositing into blood vessels [35].
Insulin-resistant individuals, such as those with metabolic syndrome or type 2 diabetes, produce more LDL. These people respond better to cholesterol-lowering drugs (statins), which block cholesterol production [36].
6) Kidney Disease
People with kidney damage and chronic kidney disease often have high LDL-C levels [37, 38, 39, 40, 41]
7) Coffee
Drinking lots of coffee may contribute to increasing LDL-C [42, 43].
According to a meta-analysis of 12 studies with a total of 1017 people, drinking coffee for 45 days was associated with an increase of 5.4 mg/dl LDL-C on average [43].
8) Lack of Sleep
In a small study of 10 healthy older women, LDL-C increased after 3 consecutive nights of sleeping only 4 hours/night [44].
In a study of 14,257 youth, shorter sleep duration in adolescence increased the likelihood of high cholesterol in young adulthood, but only among females [45].
9) Stress
In studies of 313 total adults, exposure to mental stress (solving cognitive and behavioral tasks) increased LDL-C during the task [46, 47, 48, 49].
In one of the above studies of 199 middle-aged adults, those with greater LDL-C increases during the stressful task were more likely to have elevated LDL-C 3 years later [49].
10) Medication
There are also many drugs that can increase cholesterol, including [50, 51]:
- Anabolic steroids
- Corticosteroids, drugs used to treat inflammation
- Water pills (diuretics)
- Beta-blockers
- Immunosuppressive drugs
11) Genetic Disorders
People with rare genetic disorders, such as familial hypercholesterolemia, have elevated LDL-C levels [52]. Read more about genes associated with low cholesterol below.
12) Pregnancy
LDL (including harmful small, dense LDL) is elevated during pregnancy, particularly in the second half of pregnancy. However, HDL or “good” cholesterol also increases. This increase is due to sex hormone (estrogen, progesterone) changes [53, 54, 55, 56, 57].
LDL-Cholesterol And Heart Disease
By far the biggest problem with elevated LDL-C is its accumulation in arteries. This can create fatty plaques that restrict blood flow and harden the blood vessels. Clogged arteries can become completely blocked, causing a stroke or heart attack, while hardened arteries lead to high blood pressure [1, 58, 59].
For this reason, elevated LDL-C is a direct risk factor for heart disease [60].
Even at very low levels, LDL-C was associated with artery hardening in a study of 1,779 adults [61].
Low LDL-C reduces heart disease risk. In a meta-analysis involving over 38k adults with high cholesterol, very low LDL-C (< 50 mg/dL) was associated with lower heart disease risk than LDL-C 75 – 100 mg/dL [79].
Low LDL-Cholesterol Levels
There is no lower normal limit for LDL-cholesterol. However, we do know that cholesterol levels can drop during serious illness, injury, or surgery, and gradually increase back up during recovery [62, 63].
Other conditions that can decrease cholesterol include:
- Malnourishment (low-protein diets) [64]
- Malabsorption, in conditions such as celiac disease [65]
- Anemia (iron deficiency) [66]
- Bacterial, viral, or parasitic infections [62, 67]
- Liver disease [68, 69]
- Cancer [62, 70]
- Rare genetic disorders [71, 72]
Statins, drugs used to decrease cholesterol, can decrease LDL-cholesterol levels [73, 74].
LDL-Cholesterol Genes
LDL-C levels are influenced by your genes. Here’s a breakdown of some genes that can influence LDL levels:
- Abetalipoproteinemia is a rare disease where LDL-C is almost absent. This is due to a poor ability to absorb fat (caused by a mutation in the microsomal transfer protein (MTP) gene) [75].
- Familial hypobetalipoproteinemia is another rare condition where LDL-C levels are below 50 mg/dL. The cause is a mutation of the apoprotein B (APOB) gene [76].
- Some people have reduced activity of genes that break down cholesterol (ATP-binding cassette (ABC) transporters). This can increase LDL levels and lower response to cholesterol medication [77].
- Familial hypercholesterolemia is a disease caused by mutations in several genes, including those that make the LDL receptor (LDLR) and Apoprotein B (APOB) [78]. These mutations cause problems in removing LDL from the blood, resulting in elevated LDL [78].
- In a study of 599 patients with elevated LDL, carrying an apolipoprotein 5 (APOA5) SNP was associated with smaller LDL particle size and higher oxidized LDL levels [79].
- Proprotein convertase subtilisin/kexin type 9 (PCSK9) breaks down the LDL receptor, resulting in the accumulation of LDL in the blood. Variants of PCSK9 can cause either elevated or low cholesterol [80].


