Image credit: https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0022042/?figure=1
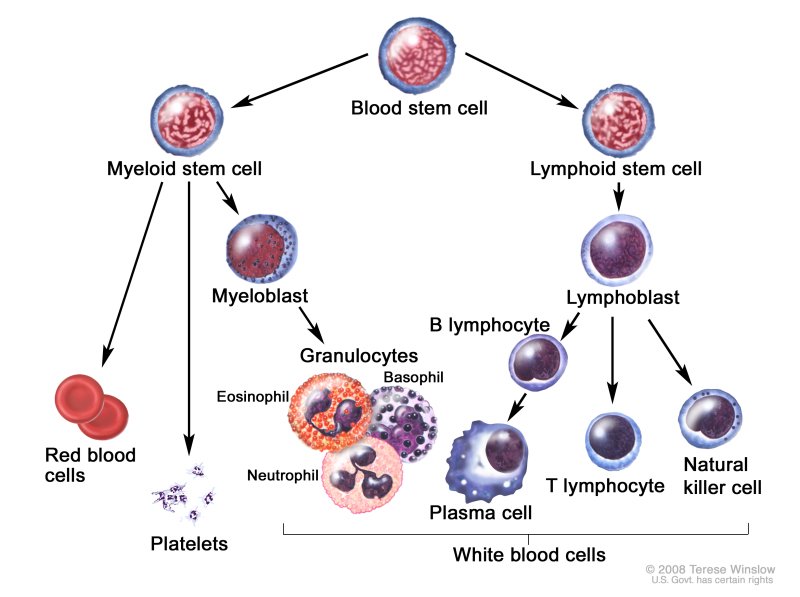
Lymphocytes are important for immune system function.
What Are Lymphocytes?
Lymphocytes are a type of white blood cells.
The different types of lymphocytes mostly differ on their site of maturation and functions [1].
There are three different types of lymphocytes: natural killer cells, B cells, and T cells.
- Natural killer cells (NK cells) kill tumor cells and virus-infected cells.
- B cells produce antibodies. The antibodies attack cells foreign to the body (bacteria, toxins, and viruses).
- T cells destroy the body’s own cells, including cancerous cells or those that have been taken over by viruses.
Lymphocytes can produce cytokines, which are small proteins that are important for immune system responses, inflammation, and infections [2].
Lymphocytes are a part of the immune system. The innate immune system responds to pathogens in a generic way but does not have long-lasting protection. The adaptive immune system responds to pathogens by using memory from previous encounters of a pathogen [3].
One gene, LSP1 (lymphocyte-specific gene 1), is expressed in lymphocytes (and other cells as well). LSP1 transduces signals between white blood cells [4].
Mature lymphocytes undergo programmed cell death. This helps preserve homeostasis and tolerance in the body [5].
Types of Lymphocytes
T cells come from the bone marrow and mature in the thymus (and sometimes the tonsils). Different types of T cells include killer, helper, regulatory, memory, and natural killer T cells.
Naive CD4+ T cells are cells that would become Th1, Th2, Th17 and regulatory T cells [6].
1) Killer (Cytotoxic) T Cells
Killer T cells, also called CD8+ T cells, can scan cell surfaces to see if they are cancerous or infected by viruses and bacteria. They destroy infected cells and help prevent autoimmune diseases.
Inappropriate killer T cell activities can lead to the persistence of the pathogens or autoimmune disease [7].
2) Helper T cells
Helper T cells, on the other hand, help start and control the body’s immune response. They help with the activation of killer T cells, maturation of B cells, and secrete cytokines. They can only work when they are activated on the surface of antigen-presenting cells [8].
Helper T cells can be categorized into different groups based on their target pathogens, e.g. Th1, Th2, and Th17.
- Th1 response is characterized by the release of interferon-gamma and is more effective against pathogens that infect inside the cells, such as bacteria and viruses [9].
- Th2 response is characterized by the release of interleukin-5 and is more effective against pathogens that infect outside the cells, such as certain bacteria and parasites [9].
- Th17 cells are inflammatory counterparts of regulatory T cells. Read this post to learn more about the Th17 immune response.
Read this post to learn more about Th1 and Th2.
3) Regulatory T cells
Regulatory T cells maintain tolerance, prevent autoimmune diseases, and limit inflammatory diseases. However, they also suppress immunity for certain pathogens and tumors [10].
4) Memory T cells
Memory T cells live for a long time after an infection is over and help the immune system remember previous infections. They rapidly multiply after re-exposure to previous infections.
There are 3 types of memory B cells, including resident, central, and effector. Memory T cells are especially important for the development of vaccines [11].
5) Natural killer T cells
Natural killer T cells help connect the adaptive with innate immune systems. They can produce cytokines and regulate immune responses against autoantigens [12].
T cell deficiency can cause damage to the immune system. Deficiency can cause hereditary conditions, severe fungal infections, cancer, and other chronic infections. T cell deficiencies are generally present in infants or toddlers [13].
B Cells
B cells mostly function in the adaptive immune system. They secrete antibodies and cytokines and mature in the bone marrow. They work with antigens, molecules that induce an immune response, to produce antibodies [14].
6) Memory B cells
Memory B cells circulate through the body to initiate a fast antibody response when they detect an antigen. They help the immune system respond faster after re-infection [14].
7) Regulatory B cells
Regulatory B cells help stop lymphocytes that can cause inflammation. They also promote the generation of regulatory T cells [15].
T cells help activate B cells, although there are some B cells that don’t need T cells for activation [14].
Abnormal B cell recognition and transformations of B cells can cause autoimmune diseases like arthritis, diabetes, lupus, multiple sclerosis, and cancers [16].
Natural Killer Cells
Natural killer cells work as part of the innate immune system. They provide fast responses to infected cells. They do not need antibodies to initiate an immune reaction [17].
Natural killer cells also play a role in the adaptive immune response to help with secondary infections. They are especially needed to help fight cancer and might show innate resistance to viruses like HIV [17].
Measuring Lymphocytes
The simplest test for lymphocytes is the white blood cell count and differential. It only needs a drop of blood to be tested by either manual count in microscopic chambers or by automated counters. Bone marrow can be used for better investigation, but blood samples are more common [18].
Lab results are commonly shown as a set of values known as a “reference range”, which is sometimes referred to as a “normal range”. A reference range includes the upper and lower limits of a lab test based on a group of otherwise healthy people.
Your healthcare provider will compare your lymphocyte count with reference values to see if it falls outside the range of expected values. By doing so, you and your healthcare provider can gain clues to help identify possible conditions or diseases.
Remember that some lab-to-lab variability occurs due to differences in equipment, techniques, and chemicals used. Don’t panic if your result is slightly out of range in the app – as long as it’s in the normal range based on the laboratory that did the testing, your value is normal.
However, it’s important to remember that a normal test doesn’t mean a particular medical condition is absent. Your doctor will interpret your results in conjunction with your medical history and other test results.
But remember that a single test isn’t enough to make a diagnosis. Your doctor will interpret this test, taking into account your medical history and other tests. A result that is slightly low/high may not be of medical significance, as this test often varies from day to day and from person to person.
Normal Reference Ranges
Lymphocyte levels can vary according to race, gender, location, and lifestyle factors.
For Caucasians, the CD4+ lymphocyte levels can range from 600 to 1000 cells/μl, while Asian and Middle Eastern populations range from 500 to 900 cells/μl [19].
CD8+ lymphocyte levels for Caucasians normally range from 400 to 660 cells/μl, while the Chinese population range from 400 to 800 cells /μl [19].
In North America, the reference ranges used during blood tests are:
- 690 – 2,540 cells/µL for CD3+ T lymphocytes (optimal is around 1,410 cells/µL)
- 410 – 1,590 cells/µL for CD4+ T lymphocytes (optimal is ~ 880 cells/µL)
- and 190 – 1,140 cells/µL for CD8+ T lymphocytes (optimal is ~ 490 cells/µL)
Other Roles of Lymphocytes
1) May Protect Against Cancer
Higher levels of Lymphocytes/T cells is indicative of the overall survival of cancer patients [20].
Specialized tumor-infiltrating lymphocytes therapy can treat liver cancer symptoms and can help stop cancer and tumors from reoccurring [21].
2) Maintaining Intestinal Health
Lymphocytes in the gut play an important role in maintaining gut homeostasis. They are also critical for the early response to intestinal infections [22].
3) Protecting Against Arthritis
Arthritic patients with high lymphocytes in the joints had less damage to the cartilage and bone than patients with low lymphocyte levels [23].
4) Affecting Blood Pressure
CD8(+), Th1, Th17, and T regulatory T cells have various effects on blood pressure [24].
Abnormalities of Lymphocytes
The conditions we discuss here are commonly associated with abnormal lymphocyte levels, but this single symptom is not enough for a diagnosis. Work with your doctor to discover what underlying condition might be causing your unusually high or low lymphocyte count and to develop an appropriate plan to improve your health.
1) Lymphoma
Lymphomagenesis is the development of lymphoma or cancer of the lymph nodes.
Lymphoma might result from uncontrolled lymphocyte growth in the body. Mutations in pathways that are involved in tumor suppression can cause the uncontrolled growth of B and T lymphocytes [25].
Hyperactivity of B-cells associated with autoimmune diseases and impaired T-cell function can also lead to lymphoma [26].
2) HIV
The most defining feature of HIV and AIDs is the decrease in number and function of T lymphocytes in the body. Most HIV-infected cells in the body are also resistant to natural killer cells [27].
In studies performed on HIV-infected patients, CD4+ T-cell was depleted the most in the gut [27].
HIV infects, causes function abnormalities, and kills CD4+ T-cells.
HIV causes T lymphocytes to undergo apoptosis (programmed cell death), causing the immune system to become weak, and not able to fight infections [28].
3) Multiple Sclerosis
Patients with multiple sclerosis (MS) have a higher amount of T cells. CD8 T lymphocytes play a part in forming MS lesions. T cells can initiate damage to the nervous system [29].
4) Type 1 Diabetes
Cytotoxic T lymphocytes may destroy cells that produce insulin, thus causing Type 1 diabetes [30].
5) Allergies and Asthma
A Th1/Th2 imbalance results in the expression of asthma and allergies. This is mostly caused by Th2 cytokines, which help maintain the inflammation response in allergic diseases [31].
6) Skin Problems
Dermatitis is a chronic inflammatory skin disease. Th2 cells and cytokines play an important part in the inflammatory response and can contribute to dermatitis [32].
7) Lymphocytosis
Abnormally high lymphocyte count (significantly higher than 3000 per mL), or lymphocytosis, can indicate a problem with the immune system. Lymphocytosis might be caused by the flu, chickenpox, tuberculosis, rubella, etc. Leukemia can also be the cause of a high lymphocyte count in the blood. Certain drugs can also cause lymphocyte levels to increase [33, 34].
Lymphocytosis does not necessarily mean that there is a problem with the immune system and may be temporary. There are rarely any symptoms that go along with lymphocytosis.
8) Lymphocytopenia
Abnormally low lymphocyte count, or lymphocytopenia, can be caused by AIDs, low bone marrow levels, steroid use, or nerve disorders like multiple sclerosis. Other, inherited disorders can also cause a low lymphocyte count [35].
Like lymphocytosis, lymphocytopenia does not necessarily indicate an immune system disorder. It could happen after a cold or another common infection. Severe stress, intense physical exercise, or malnutrition can also be the cause [36].
How to Modify Lymphocyte Levels
How to Increase Lymphocytes
Usually, you will only know your lymphocyte levels if the doctor has requested a specific blood test. The most important thing is to work with your doctor to diagnose and treat the underlying health problems that may be causing your abnormal lymphocyte count.
Depending on the condition, your doctor may prescribe the following therapies:
- Antiretroviral combination therapy for HIV
- Antibiotics, antivirals, antifungals, or antiparasitic drugs for different types of infections
- Gamma globulin to prevent infections in people with B-cell lymphocytopenia
- Bone marrow stem cell transplant for some cancers (such as leukemia, multiple myeloma, and some types of lymphoma)
If a drug is causing your low lymphocyte levels (e.g., immunosuppressants and steroids), your doctor may reduce its dose or discontinue it.
People with low lymphocyte levels should boost their immune system by eating a nutrient-rich diet providing sufficient proteins, vitamins, and minerals. Doctors may prescribe a special diet for people with a weakened immune system.
Additionally, it’s important to prevent infections by:
- Frequently washing hands with soap or sanitizer
- Avoiding crowded areas
- Avoiding contact with ill people
- Staying away from animals
- Avoiding activities that may cause cuts, scrapes, or nicks on the skin
The additional supplements listed below may help you modify your lymphocyte levels. Discuss with your doctor if they may be helpful in your case. None of them should ever be implemented in place of what your doctor recommends or prescribes!
- Reishi mushroom supplementation for 28 days in 40 football players stimulated T cell formation [37].
- Holy basil (Ocimum sanctum) herb extract increased T cells and cytokines after 4 weeks supplementation in 40 healthy volunteers [38].
- Creatine (Cr) displays antioxidant activity and it protects white blood cells against oxidative damage. Creatine and its by-product, creatinine, both help protect lymphocytes and help prolong their lifespan [39].
- Vitamin A: Vitamin A has a direct effect on T lymphocytes and their activation. It also stabilizes Th1 cells. Vitamin A deficiency, although rare, can cause immune system problems [40].
- Vitamin D: This vitamin affects intraepithelial lymphocyte development. Deficiency of Vitamin D is linked to autoimmune and infectious diseases [40].
How to Decrease Lymphocytes
The most important thing in case of high lymphocyte levels (lymphocytosis) is to identify and treat the underlying cause (most commonly infections and leukemia). Lymphocytosis usually goes away after resolving the condition that caused it [41].
Because high lymphocyte levels are often caused by infections, the main preventive strategy is to reduce their risk by [42]:
- Frequently washing hands with soap or sanitizer
- Avoiding contact with ill people or sharing objects with them
- Disinfecting surfaces and commonly used objects
The complementary strategies listed below may help you lower your lymphocyte levels. Discuss with your doctor if they may be helpful in your case. None of them should ever be implemented in place of what your doctor recommends or prescribes!
1) Drugs
The following drugs may lower your lymphocyte count if you are already taking them for some other health condition, but never start taking them or increase your dose for this purpose. Always follow the treatment plan prescribed by your doctor.
- Steroids such as glucocorticoids inhibit lymphocyte proliferation. Synthetic steroids inhibited both circulating T and B cells [43].
- Adalimumab (Humira) affects the levels and function of T lymphocytes in rheumatoid arthritis patients. However, there are conflicting reports of whether or not the drug increases or suppresses lymphocytes. The effects are also temporary [44].
- Immunosuppressant drugs have lowering effects on the T and B lymphocyte levels in the blood. In one study of 60 patients, cyclophosphamide given with azathioprine decreased the T lymphocyte proportion. In turn, prednisone, cyclophosphamide, methotrexate, mycophenolate mofetil, and azathioprine decreased more than 60% of B lymphocytes in mice [45, 46].
- Pentoxifylline inhibits the early steps of T lymphocyte activation [47].
2) Supplements
- Echinacea: in healthy humans, Echinacea alone lowers IL-2 (a Th1 cytokine) and may inhibit T cell proliferation. On the other hand, it increases IL-10 (a Th2 cytokine) and can lower the inflammatory response [48].
- Fish oil: feeding mice with fish oil impaired the activity of T cells against a cold virus but improved lymphocyte proliferation [49].


