In addition to well-established causes, dysfunction in other pathways or organ systems may contribute to thyroid disorders. These include microbiome impairment, stress, toxin exposure, nutritional deficits, and more. Read this post to learn more about the thyroid hormones control, factors that may reduce them, and what you can do about it.
What are Thyroid Hormones?
The thyroid gland produces and secretes thyroid hormones T3 (triiodothyronine) and T4 (thyroxine).
T3 contains three iodine atoms and is created from the breakdown of T4. The breakdown of T4 is encouraged by the Thyroid Stimulating Hormone (TSH).
T4 is synthesized from the amino acid tyrosine, found in thyroglobulin (a protein created in the thyroid). It contains four iodine atoms.
Lack of T3 early in human development causes stunted growth.
T3 is very important in increasing energy production.
Roles & Functions
- Breathing
- Energy production
- Heart rate
- Cognitive function
- Mood
- Body weight
- Muscle strength
- Menstrual cycles
- Body temperature
- Cholesterol levels
- Growth and development
- Intestinal flow
- Digestion
If you notice any of the symptoms described below and suspect a thyroid disorder, seek medical attention. Most thyroid conditions can be successfully treated if diagnosed on time.
Hyperthyroidism Symptoms
Hyperthyroidism (too much T3 or T4) symptoms include:
- Sweating or sensitivity to high temperatures
- Hair loss
- Faster heart rate
- Diarrhea
- Weight loss
- Missed or light menstrual periods
Hypothyroidism Symptoms
Hypothyroidism (insufficient T3 or T4) symptoms include:
- Trouble sleeping
- Tiredness and fatigue
- Difficulty concentrating
- Depression
- Sensitivity to cold temperature
- Frequent, heavy periods
- Slow heart rate
- Weight gain
- Dry skin and hair
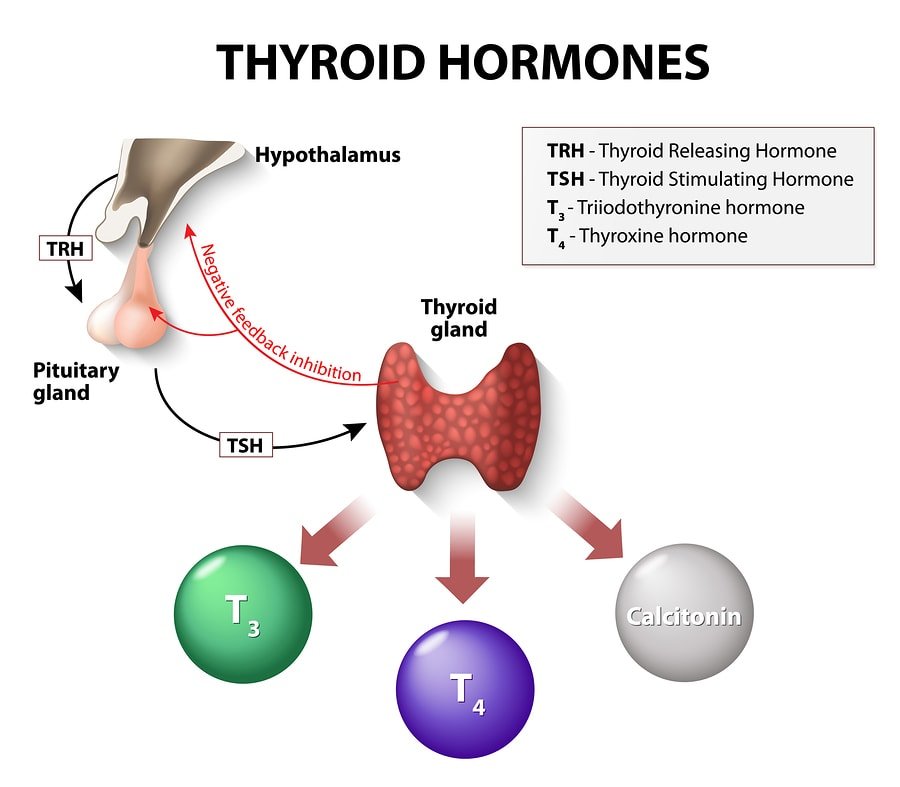
The Hypothalamus-Pituitary-Thyroid (HPT) Axis
The hypothalamus, pituitary, and the thyroid gland (also called the hypothalamic/pituitary/thyroid or HPT axis) control thyroid hormone levels [1].
Thyrotropin-releasing hormone (TRH) made in the hypothalamus binds to the receptors in the pituitary, causing it to release the thyroid-stimulating hormone (TSH), which then stimulates T4 production.
If there is too little of the thyroid hormones in the bloodstream, the hypothalamus signals the pituitary gland (via TRH) to produce TSH for the thyroid to release more T3 and T4.
Once there is enough of these hormones, the hypothalamus is signaled to stop the release of TRH and the cascade of actions to increase T3 and T4.
High free T4 and free T3 levels signal the pituitary to adjust TSH and TRH levels.
Somatostatin and dopamine from the hypothalamus also reduce TSH levels, thus reducing thyroid hormones.
Conversion of T4 to the More Active T3
Both T3 and T4 are produced in the thyroid gland, although T3 is much more potent than T4.
In the blood, T4 levels are around 45 fold higher (90 nM) than T3 (2 nM).
Most T3 is produced by removing iodine from T4 in a process that requires selenium [2].
The total activity of T3 thyroid hormone in the body depends on the enzymes that converts T4 to T3, which are found outside of the thyroid:
- Type 1 deiodinase, which generates T3 for circulation, is found in the liver and kidney.
- Type 2 deiodinase converts T4 to T3 within the cells of the brain, pituitary, and brown fat tissue.
- Type 3 deiodinase, found in the placenta, brain, and skin, leads to the generation of rT3
Carrier proteins bind to most thyroid hormones, leaving only a very small fraction available. These include thyroxine binding globulin (TBG), albumin, and thyroid binding prealbumin.
Thyroxine Binding Globulin is made by the liver [3].
- 99.97% of T4 is bound, and 0.03% is free.
- 99.7% of T3 is bound and 0.3% of T3 is free.
Factors That May Reduce Thyroid Function
Most of the below factors are not established causes of hypothyroidism. According to preliminary research, they may play a role in this complex condition, but the evidence is inconclusive. If you recognize one or more of these factors in your case, it doesn’t mean you have hypothyroidism. If you’re suspecting a thyroid condition, work with your doctor to get adequate diagnosis and treatment.
1) Altered Gut Bacteria
Used thyroid hormones are deactivated by the liver and then excreted into the gut as part of bile. In the stomach, the thyroid hormones are absorbed and reabsorbed, so digestive problems reduce the levels of thyroid hormone reabsorption [4].
Gut bacteria also influence thyroid hormone levels. In rats, gut bacteria convert the deactivated thyroid hormone back into T3 and causes recycling of the T3 that would be eliminated [5].
Treatment with antibiotic increased blood T4 and rT3, but did not affect T3 levels [5].
2) Stress
Stress can both reduce and increase thyroid hormones, based on various factors. Acute stressors reduce TSH levels and thereby T4 levels [6, 7].
This makes TSH levels a less accurate marker to screen for hypothyroidism in the presence of stress.
Stress types decreasing thyroid hormones:
- In mice, repeated foot-shock stress increased cortisol, while reducing T3 and T4 [8].
- Inescapable tail shock stress reduced thyroid hormones in rodents [9, 10].
- Restraint (immobilization) stress decreased blood T3, increased blood rT3, and reduced T4 to T3 conversion in the liver and kidney. Removing the adrenals or blocking cortisol completely prevents the changes in thyroid hormones in response to stress [11].
Stress hormones reducing thyroid hormones:
- Chronic HPA axis activation inhibits TSH and T4 to T3 conversion [12].
- Cortisol inhibits TRH and the conversion of T4 to T3 in non-thyroid tissues in rats [13, 14, 15].
- CRH and cortisol both reduce blood T3 and T4 concentrations [16].
- Administration of dexamethasone (a synthetic cortisol) suppress TSH levels in rats [14].
3) Inflammation
In rats, injection of LPS (a bacterial toxin) suppresses the production of TRH, TSH, and T3 levels, while increasing CRH and cortisol levels. However, blocking the CRH and cortisol increase does not prevent the reduction in TRH and TSH levels due to LPS-induced inflammation [9].
Chronic inflammation in mice reduces TRH production in mice and rabbits [17, 18].
Injection of IL-1, TNF, and IFN-gamma either in the blood or the brain results in a fall of blood TSH levels in rats. This may be because TNF reduces TRH production in rat hypothalamus [19, 20, 21].
Proinflammatory cytokines inhibit T4 to T3 conversion in a cell-based study [22].
TNF-alpha inhibited TSH activation of human thyroid cells in a cell-based study [23].
Blood IL-2 levels are increased in some patients with primary hypothyroidism [24].
4) Low Leptin or Leptin Resistance
Overfeeding newborns during the breastfeeding period may lead to obesity, leptin resistance, and lower thyroid hormone during adulthood [25, 26].
High leptin levels in newborn rats lead to leptin resistance and hypothyroidism in the hypothalamus at 30 days of age and at adulthood. In these animals, acute cold at 30 days old normalized leptin levels and restored leptin sensitivity in the hypothalamus. In addition, cold exposure further increased thyroid hormones [27].
Fasting reduces leptin and therefore reduces TRH, TSH production, T3, T4, and liver enzymes that convert T4 to T3 [28].
In addition, some leptin-resistant humans have low T4 and normal TSH [29].
A leptin analog increased FT3 and FT4 in leptin-deficient children, and the reverse decreased T3 and T4 levels in people on a low-calorie diet [29, 30].
However, leptin administration does not reverse changes in thyroid hormone levels in acute fasting [31].
5) Environmental Toxins
Environmental toxins like polychlorinated biphenyls PCBs, polybrominated diphenyl ethers (PBDE), and other hormone disruptors, interfere with thyroid function [32, 33].
6) Fluoride
Fluoride was given to hyperthyroid patients to lower thyroid hormones in the past.
In a study of Indian school children, there were significant differences in TSH and thyroid hormone levels between two groups of students that are exposed to different levels of fluoride [34].
In a study of over 400 participants, “fluoride had impacts on TSH and T3 hormones even in the standard concentration of less than 0.5 mg/L” [35].
In zebrafish, mice, and rats, fluoride causes thyroid dysfunction, which could be ameliorated by taurine and calcium [36, 37, 38].
Nutrient Deficiencies That May Reduce Thyroid Hormones
7) Iodine
Iodine is required for the production of thyroid hormones. Iodine deficiency is a major cause of hypothyroidism, especially in developing countries [39].
However, getting more than 400mcg is problematic and may also contribute to thyroid disorders [40, 41].
8) Selenium
Selenium is needed to convert T4 to T3. It stimulates thyroid function and protects against autoimmune thyroid conditions. Selenium deficiency contributes to hypothyroidism [42, 43, 44].
Selenium also increases chromium excretion, so pay attention to your daily chromium intake in case you’re supplementing.
9) Iron
Iron is needed for thyroid peroxidase function, which is important in the synthesis of thyroid hormone [45].
Chronic anemia due to iron deficiency is a well-known factor that impairs thyroid function [46].
10) Vitamin A
Vitamin A can bind to thyroid hormone receptors.
In a study on obese women, vitamin A increased T3 and lowered TSH [47].
Vitamin A-deficient rats had two times lower thyroid hormones in one experiment [48].
Complementary Approaches to Improve Thyroid Function
if you’re experiencing symptoms of a thyroid disorder, it is important to consult with your doctor ASAP to ensure you get adequate medical care. They may suggest adding the complementary approaches mentioned below – but they should not be used to replace conventional medical treatment.
Keeping the discussed contributing factors in mind, in addition to suggested treatment and complementary approaches, you may want to:
- Maintain Circadian Rhythm and Leptin Sensitivity
- Correct Nutritional Deficiencies
- Correct Intestinal Gut Bacteria Imbalance and Gut Infections
- Reduce Inflammation
- Reduce Stress
- Reduce Environmental Toxins

