You’ve heard it in a dozen textbooks: the mitochondria are the powerhouse of the cell. They are the part of the cell responsible for turning the food into energy for the body. Read on to learn more about the mitochondria, how they work, and how they can affect your health.
What Are Mitochondria?
Definition
The mitochondrion (plural mitochondria) is a membrane-enclosed organelle responsible for the conversion of fats and carbohydrates (glucose) into usable forms of energy for the body [1, 2].
The main function of the mitochondria is to produce ATP, the main source of energy used by all cells. ATP is used for all the necessary activities of the cell, and we must eat to replenish ATP production [2].
Mitochondria use oxygen to produce ATP in a process known as aerobic or cellular respiration. This reaction uses oxygen and produces carbon dioxide, which we exhale through our lungs [2].
The number of mitochondria per cell varies with every cell type. As the energy demands of a cell increase, for example in muscle cells, the number of mitochondria will also increase. This allows for more energy production and usage in active cells [2].
Aside from the production of energy, mitochondria play a vital role in monitoring calcium levels, which helps balance energy demand and production in the cell [3].
It is also responsible for initiating the destruction of old and faulty cells, a process called apoptosis. This is necessary to make room for growth and regeneration of cells after injuries and to prevent cancer growth [4, 5].
Byproducts of mitochondrial activities accumulate and produce free radicals. This causes oxidative stress, a leading cause of almost all age-related diseases [6].
Improper mitochondrial function leads to the buildup of waste and prevents faulty cells from being removed from the body. This can result in tumor growth and cancer [5].
The mitochondria are the target of a number of new promising therapies for cancer, heart failure, insulin resistance, and neurodegenerative disorders [5].
Since energy is central to life, some researchers have argued that improving mitochondrial function could be directly beneficial to physical and mental health.
Mitochondrial DNA
The majority of the human genome, which is all of the DNA in an individual, is packaged into 23 pairs of chromosomes in the nucleus of the cell. In addition to nuclear DNA, humans also carry a specific set of 37 genes that are only found in the mitochondria [7].
Mitochondrial DNA (mtDNA) is collected into a single circular chromosome. Each mitochondrion carries 2 to 10 copies of this chromosome [8].
Mitochondrial DNA mainly codes for proteins that are needed for mitochondrial function. In contrast, nuclear DNA codes for proteins that are required to activate the synthesis of mitochondrial proteins [8].
The 23 pairs of chromosomes in the nucleus are inherited from both parents after undergoing recombination, a process that makes you unique [9].
Conversely, mitochondrial DNA can only be inherited from the mother. Paternal mtDNA is believed to be broken down and discarded after the sperm enters the egg [8].
Origin of the Mitochondrion
Some of the first living organisms on earth were single-celled prokaryotic organisms like bacteria. Human beings are eukaryotic organisms, meaning that we are composed of eukaryotic cells. It is hypothesized that eukaryotic cells originated from prokaryotic cells [10, 11].
Prokaryotes differ from eukaryotes in a number of ways [10]:
- Prokaryotes do not have internal compartments (organelles).
- DNA is circular, not linear like in eukaryotes.
- Prokaryotes do not have a nucleus, and thus their DNA floats freely within the center of the cell, while eukaryotic DNA is packaged into the nucleus of each cell.
- Prokaryotic DNA is simpler than eukaryotic DNA.
- Prokaryotes replicate by splitting in half and producing 2 identical copies (binary fission).
Due to their many similarities, the mitochondria are thought to have evolved from ancient oxygen-using prokaryotic cells like bacteria [10, 11].
- Structurally, the mitochondria resemble bacteria.
- It is composed of a double membrane through which ATP is synthesized, similar to bacterial ATP production.
- It carries its own circular DNA.
- The sequence of mitochondrial DNA strongly resembles the sequence of DNA in modern prokaryotes (Rickettsia prowazekii).
- Like prokaryotic organisms, the mitochondrion can replicate itself within the cell by binary fission.
The most widely accepted theory that explains these features is the endosymbiotic theory. This theory suggests that ancient prokaryotic organisms that produced energy-using oxygen accidentally fused with eukaryotic cells that did not use oxygen. The two cells mutually benefit from working together as an individual unit (endosymbionts) [10, 11].
The ability to use oxygen for energy proved to be favorable to the survival of both of the cells. Over time, the fused cells evolved into modern eukaryotic organisms. The mitochondria are thought to be a remnant of this original prokaryotic organism [11].
Mitochondria Structure
Characteristics
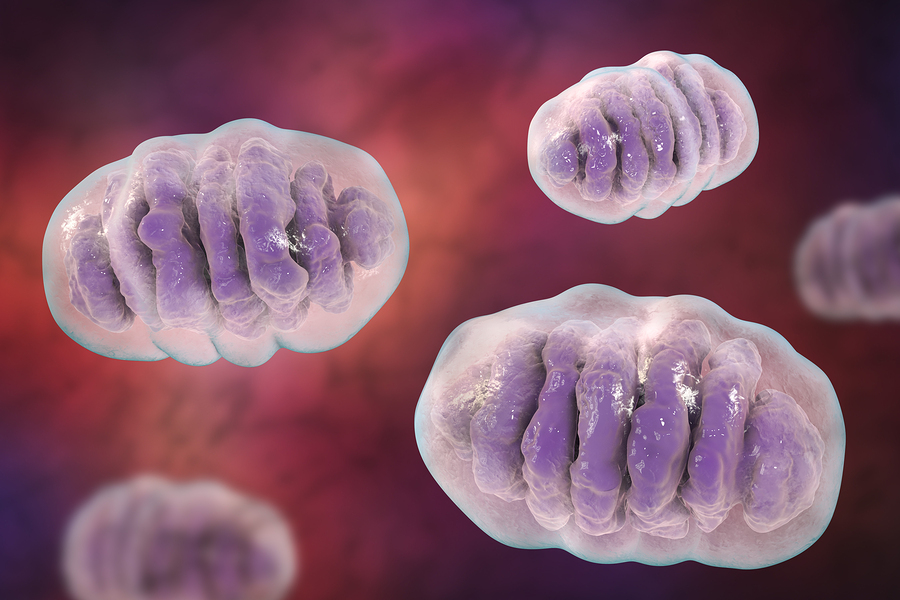
The structure of the mitochondrion is highly unusual, which is conducive to its function as an ATP-making machine [1].
The mitochondrion is enclosed by a double membrane and the inside of the organelle is called the matrix. The inner membrane folds multiple times into structures called cristae. The ATP-making proteins are located between these two membranes and movement of ions across the inner membrane powers these proteins. The presence of the cristae increases the surface area available for ATP production [1, 3].
The matrix contains a copy of the circular DNA and proteins responsible for mediating mitochondrial activity. These include proteins that create ATP, stimulate mitochondrial division and the fusion of mitochondria, metabolize molecules, and induce apoptosis [1].
Mitochondria can undergo division (fission) and fusion. Mitochondrial division increases the number of mitochondria by dividing one mitochondrion in two or producing a new mitochondrion from a small fragment of the original mitochondrion [3].
Mitochondrial fusion occurs when two mitochondria fuse together, forming an elongated structure. This usually occurs when there is damage. By fusing together, mitochondria can overcome the dysfunction allowing the two semi-damaged mitochondria to work as one fully-functioning mitochondrion (complementation) [3].
Mitochondria Vs. Chloroplasts
The structure and function of mitochondria are very similar to chloroplasts. Chloroplasts are found within plants and some algae. Like mitochondria, they:
- have their own double membrane
- have their own set of DNA and RNA
- provide energy to the cell
- have similar sets of enzymes and proteins
Unlike mitochondria, chloroplasts use sunlight to make energy for the plant through a process known as photosynthesis.
Function of the Mitochondria
The mitochondria are responsible for the conversion of fats and carbohydrates into ATP, the energy currency of the cell. In addition, mitochondria can induce cell death when necessary, manage calcium levels, and break down carbon-based molecules [3, 12].
Byproducts of normal mitochondrial function accumulate and produce free radicals. This leads to oxidative stress, which is a leading cause of almost every serious age-related disease [12].
1) The Powerhouse of the Cell
The most significant role that mitochondria play is the production of ATP. A series of biochemical reactions both inside and outside of the mitochondria results in the production of ATP through a process called oxidative phosphorylation. Aside from having a normal cellular function, these reactions require food and oxygen for energy production [13].
Fats, carbohydrates, and proteins all provide the body with different amounts of ATP when broken down [12].
Carbohydrates, which are converted to glucose molecules, are the quickest to break down and generate 34 to 38 molecules of ATP for every molecule of glucose that undergoes respiration. They are the body’s preferred form of energy [14].
Fats are used for energy when glucose levels are low. A single molecule of palmitic acid, a common saturated fat, can produce 130 molecules of ATP. However, the breakdown of fats (lipolysis) is a much more complex process, and it can take up to 72 hours to digest a fatty meal [15].
Proteins are only used for energy when the body is starved [15].
What Is Cellular Respiration?
There are 3 stages in cellular respiration [16]: glycolysis, Krebs cycle, and oxidative phosphorylation.
Glycolysis
Once carbohydrates or glycerol from fats is broken down into glucose molecules, they undergo a series of reactions called glycolysis [3].
- Glycolysis occurs outside of the mitochondria, in the cytosol of the cell.
- It is an anaerobic process, meaning that it does not need oxygen to occur.
- It results in the net production of 2 molecules of ATP, 2 molecules of NADH+, and 2 molecules of pyruvate.
Glycolysis alone does not generate enough energy for the cell, but the products of glycolysis travel into the mitochondria where they pass through the Krebs cycle, also known as the tricarboxylic-acid cycle (TCA) or citric acid cycle [3].
- Pyruvate and NADH diffuse into the mitochondria (matrix).
- Pyruvate undergoes a reaction that generates 2 intermediary molecules called acetyl-CoA.
- Carbon dioxide is produced as a waste product and can be excreted through the lungs.
Fats are converted into glycerol and fatty acid tails. Glycerol can be broken down into glucose in the cytosol, which then enters the cellular respiration pathway at glycolysis. The fatty acid tails undergo a series of reactions through a process called beta-oxidation. This produces acetyl-CoA, which can enter respiration at the second stage [3].
In the event of starvation (absence of both carbohydrates and fats), amino acids from proteins are converted to small carbon-based molecules in the mitochondria. These molecules can enter the respiratory pathway at the Krebs cycle to produce ATP. This is harmful because the proteins used to provide energy are taken from our bones, muscle, and skin [16].
Krebs Cycle
The Krebs cycle is the stage in which the glucose is completely converted to carbon dioxide using oxygen (oxidation). It involves a series of reactions using the acetyl-CoA previously generated. Acetyl-CoA produced from the breakdown of fats enters respiration at this stage. The objective of the Krebs cycle is to produce high-energy molecules that can later be used to generate a larger amount of ATP [14].
- Acetyl-CoA enters the Krebs cycle in the mitochondrial matrix.
- Four reactions requiring oxygen result in the net yield of 2 ATP, 6 NADH, and 2 FADH2 molecules.
NADH and FADH2 are high-energy molecules that provide the greatest source of energy for ATP production. They are used in the third stage of respiration, oxidative phosphorylation [14].
Oxidative Phosphorylation
This stage of respiration is the most important as it generates the largest amount of ATP. This is where the structure of the mitochondrion plays a large role. Also, this process is the reason we need oxygen to survive [17, 3].
Between the outer and inner membranes of the mitochondria exists a small space called the intermembrane space. A group of mitochondrial enzymes and protein complexes line the inner membrane, forming a structure called the electron transport chain. Oxidative phosphorylation occurs in two steps: electron transport and chemiosmosis [17].
Electron Transport Chain [17]:
- Six NADH and two FADH2 undergo chemical reactions and donate their electrons to the first of the protein complexes in the electron transport chain.
- NADH becomes NAD+.
- FADH2 becomes FAD.
- Electrons are passed from complex to complex along the chain.
- As electrons pass from one protein complex to the next, they generate energy.
Chemiosmosis [17]:
- The energy generated by passing electrons down the transport chain is used to pump H+ ions from the inner mitochondrial matrix into the intermembrane space.
- The H+ ions accumulate between the two mitochondrial membranes.
- At some point, the amount of H+ ions within the inner membrane space is much larger than the amount of H+ within the mitochondrial matrix, creating a chemical gradient across the inner membrane.
- H+ ions flow back into the matrix down their concentration gradient, releasing a large amount of energy.
- The final enzyme of the electron transport chain, ATP synthase, harvests the energy generated by the flow of H+ ions into the matrix.
- ATP synthase uses this energy to generate 34 to 38 ATP molecules and 6 H2O molecules.
The purpose of oxygen in the respiratory process is to pick up the H+ ions that flow back into the cell and form water molecules. If we had no oxygen, the H+ ions would remain within the mitochondrial matrix. This would diminish the gradient created across the inner membrane because there will be H+ ions on both sides of the membrane. This will prevent chemiosmosis and. ultimately, there will be no energy for ATP production [17, 3].
2) Triggering Cell Death
Mitochondria play a major role in initiating cell death when the cell is either damaged or aged. This is useful to focus energy production on cells and tissues that have higher energy demands. Cellular death also prevents the spread of mutated and faulty cells. The process of cellular suicide is called apoptosis, which is largely mediated by the release of “suicide” proteins from the mitochondria [4, 18].
When only a mitochondrion is damaged, mitochondria can destroy themselves, by a process called mitophagy, leaving the cell and other mitochondria intact [18].
The electron transport chain, found in the inner membrane of the mitochondrion, often leaks free radicals, or reactive oxygen species (ROS). While free radical production is normal, it can lead to harmful oxidative stress in the cell. Free radicals react with many other substances in the cell, leading to DNA damage and the destruction of many vital proteins [4, 18].
The buildup of oxidative stress is linked to over 200 human diseases. Apoptosis, or programmed cell death, prevent the accumulation of free radicals. Mitochondria can respond to apoptotic signals inside (intrinsic pathway) and outside of the cell (extrinsic pathway) [4, 18].
Aside from free radicals, certain proteins can bind to receptors on the surface of the cell and initiate apoptosis. These are called death signals, and they are released in response to DNA mutations, radiation, or starvation of nutrients [4, 18].
When death signals bind to their receptors on the cell, they cause a number of chemical reactions that lead to changes in the mitochondrial membrane. This leads to the movement of proteins into the mitochondrial matrix, releasing a protein called cytochrome C from the inner membrane [4, 18].
Cytochrome C is one of the proteins in the electron transport chain. When released from the mitochondrion, the cell must undergo apoptosis. It is the determining factor of cell death [3, 18].
The destructive events of apoptosis are carried out by caspase enzymes. Caspases exist in their inactive form in every cell. When cytochrome C is released, a series of chemical reactions activate the caspase enzymes. Caspases cleave, or cut up, the different proteins in the cell. As the process goes on, the caspases lead to complete destruction of the cellular contents [18].
3) Breakdown of Organic Molecules
The mitochondria contain enzymes that break down many different molecules to be used for energy in the cellular respiration pathway. These enzymes also produce intermediary molecules that are made up of only one carbon atom. These 1-carbon-based molecules are highly reactive and can interfere with natural cellular activities [19, 20].
Inside mitochondria, 1-carbon molecules are converted into different amino acids that are needed for ATP and protein production. Vitamins B9, B12, B6, and B2 provide the carbons needed to carry out these reactions. Deficiencies in B vitamins are linked to age-related diseases like Alzheimer’s disease, cardiovascular disease, and cancer [19, 21].
The production of haem groups, the structural core of hemoglobin, found in red blood cells, is an example of one important substance produced by 1-carbon metabolism in the mitochondria. Hemoglobin is an iron-containing protein that allows for oxygen and carbon dioxide to be carried in the blood and transported around the body [12].
The 1-carbon-based molecules are exported from the mitochondria to produce some of the building blocks of DNA. This occurs in the jelly-like fluid that fills the inside of a cell (cytoplasm), where the products can either be moved to different parts of the cell as needed or exported to other tissues [21].
The mitochondria also form part of the urea cycle, the process in which nitrogen atoms from different molecules are excreted through the body as urea. Urea is the main substance found in urine, producing its yellow color [12, 22].
Therefore, the mitochondria prevent the disruption of normal cellular function, participate in the removal of waste products, and provide precursor molecules needed for other reactions.
4) Calcium Balance
Mitochondria monitor calcium levels in the cell to coordinate energy production with energy demand. Calcium levels increase in the cell for the activation of almost any biochemical pathway. Activating a cell, in turn, requires energy, so mitochondria will have to increase ATP production [3].
When calcium enters the cell, the concentration of calcium increases outside of the mitochondrial matrix. This creates a concentration gradient that drives the flow of calcium into the matrix. Protein channels that allow calcium entry is located on the inner membrane and open in response to high intracellular calcium concentrations [3].
In muscle cells, calcium entry results in increased mitochondrial production. This allows for the energy supply to meet the energy demand of that tissue [3].
Takeaway
The mitochondria are among the most unusual cellular organelles that we can’t survive without.
Scientists hypothesize mitochondria are the remnants of ancient, single-celled organisms. They have their own DNA, which is inherited maternally and more similar to the DNA of viruses than of humans.
Mitochondria produce the main source of cellular energy, ATP. They also help recycle parts of cells that can be reused while removing cells that are old and damaged beyond repair.
But since the mitochondria use oxygen, their byproducts can cause oxidative stress. When mitochondria break down, free radicals and cellular waste can build up and cause widespread harm. Some experimental, new therapies aim to reverse this process.
