If your chronic health issues all started/worsened after a major traumatic event in your life, you may have some brain chemistry changes similar to those with PTSD, even if you have not officially been diagnosed with it. Understanding PTSD and how these traumas led to your stress responses being stuck on (adrenal fatigue) and natural ways to deal with it might help resolve your health problems.
What Is PTSD?
Post-traumatic stress disorder (PTSD) is a psychiatric disorder marked by psychological symptoms, such as re-experiencing an event, dysfunctional fear memories, and physical symptoms such as anxiety and increased heart rate. These symptoms usually persist for longer than one month [1, 2].
PTSD develops from experiencing a traumatic event (e.g., a terrorist attack, military combat, a natural disaster, etc.) that has a more significant impact than that of daily stressors [1].
PTSD is common among military veterans, with around 20% of combat-exposed soldiers developing and suffering from PTSD [3].
The National Comorbidity Survey Replication has estimated that the lifetime prevalence of PTSD is 9.7% among women and 3.6% among men. More than 60% of the people experience at least one traumatic event in their life [4].
Symptoms and Diagnostic Criteria Of PTSD
PTSD is diagnosed on the basis of a long list of criteria by specialized psychiatrists at least one month following a traumatic event. However, the symptoms may not appear until several months or even years later. The main symptoms include:
- Re-experiencing the traumatic event as flashbacks or nightmares
- Experiencing emotional numbness and avoiding specific places, people, or activities that remind of the traumatic event
- Having sleeping difficulties or even insomnia and inability to concentrate, feeling jumpy, or being easily irritated and angered [5]
Many people with PTSD also have other psychiatric disorders including major depression and anxiety [5].
Individuals with PTSD are more likely to use drugs, experience impairments in psychosocial functioning, and have suicidal behaviors than the general population [6].
Consult a doctor for a proper diagnosis if you experience any of these symptoms after a traumatic experience.
Causes of PTSD
1) Excess Adrenaline and Noradrenaline
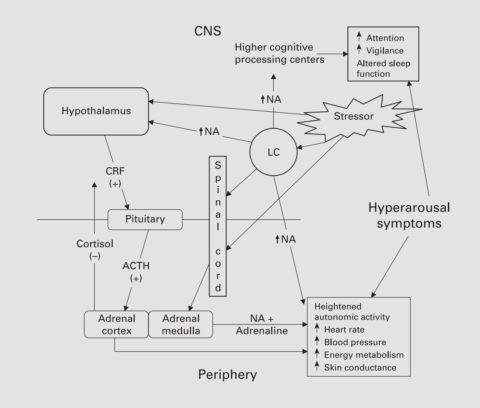
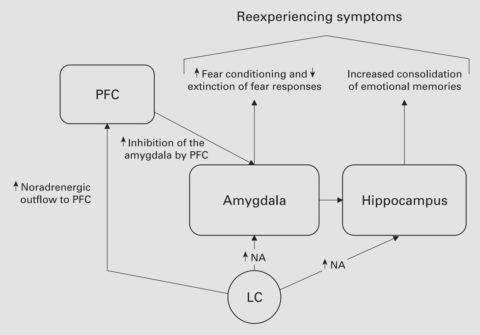
The adrenaline and noradrenaline receptors stimulate brain activity and fight-or-flight (sympathetic) autonomic responses through the amygdala and hypothalamus, which are responsible for stress and fear [7].
(figure source: [7])
Elevated noradrenaline levels in certain brain regions (prefrontal cortex and hippocampus) following trauma predicted PTSD symptoms in a study in mice [8].
Noradrenaline plays a role in the memory encoding of negative events. An imbalance of noradrenaline leads to re-experiencing traumatic memories and maintaining hyperarousal, both common symptoms of PTSD [9, 7].
A study on 44 patients showed an overabundance of adrenaline and noradrenaline in the urine of those with PTSD and other mental disorders [10].
Noradrenaline levels were also increased in PTSD patients without other diseases [7].
It is not fully understood why some people develop PTSD following trauma while others have no psychiatric effects or experience other disorders such as depression, substance abuse, or somatization.
There is evidence that some people may be genetically predisposed to the development of PTSD after a traumatic event [11].
Genes that encode adrenoreceptors may play a role in PTSD, since substances that interact with α2-adrenoreceptors (like yohimbine) increase their activity leading to fear extinction and increasing anxiety and PTSD symptoms severity. Also, substances that interact with β-adrenoreceptors (like propranolol) inhibit fear memory reconsolidation [7].
The noradrenaline transporter (NET) is a potential noradrenaline target for PTSD treatment. NET availability is reduced in the brain (locus coeruleus) of PTSD patients with an increase in the severity of anxious arousal symptoms [12, 11].
2) Decreased Serotonin Receptors in The Brain
The serotonergic (5-HT) receptors are involved in cognition, emotional processing, and behavior [13].
Substances that activate 5-HT can induce anxiety attacks and trauma-related flashbacks in PTSD patients [6].
Fear and threat responses have been linked to 5-HT signaling in the amygdala, an area of the brain important in fear and stress responses [14].
A study involving brain scans of 16 patients with PTSD found decreased serotonin receptors in the amygdala when compared to those of 16 healthy people [15].
Genetics also plays an important role in PTSD caused by a serotonin imbalance.
In a study on over 1.2k people who experienced both childhood and adult traumatic events, those who carried 1 or 2 copies of the S (short) allele for 5-HTTLPR, a common polymorphism found to increase the serotonin transporter SLC6A4, had a higher risk of PTSD [16].
3) Increased Substance P Receptors in The Brain
Substance P is a neuropeptide that plays an important role in response to extreme stressors that could compromise biological integrity. Its receptor, neurokinin 1 (NK1), is located within brain areas involved in stress and anxiety [17].
Increased substance P is involved in both major depression and PTSD. Substance P responds acutely to psychological stress in humans [18].
In the above-mentioned study on 16 patients with PTSD, they also had increased substance P receptors in the amygdala. From this study, we can conclude that the coupling of the serotonin and substance P pathways is important to the propagation of anxiety and fear symptoms in PTSD [15].
4) Overabundance of Glutamate
In a study of 110 people, elevated blood levels of the excitatory neurotransmitter glutamate were found compared with healthy controls 3 months after experiencing traumatic accidents. Glutamate plays a part in learning and memory pathways in the brain [19].
Overstimulation of neurons in the brain through glutamate can cause a malfunction in learning and memory pathways. Studies showed a positive relationship between the severity of PTSD symptoms and elevated glutamate levels [19].
After a traumatic event, dissociative symptoms predict the development of PTSD. Stress increases glutamate, which in animals influences behavior and induces plasticity of the brain that may have long-lasting effects on brain function and behavior [20].
A recent study suggests that a drug that reduces glutamate also decreases the effects of the NMDA antagonist, ketamine, in humans. Thus, drugs that decrease glutamate might help patients with dissociative symptoms due to PTSD [20].
5) Low GABA Levels
In a study of 27 PTSD patients suffering from insomnia, low levels of the inhibitory neurotransmitter GABA, a molecule that is crucial to preventing the hyperarousal symptoms of PTSD, were associated with poor sleep quality [21].
In addition, a study on over 100 road traffic accident victims found that those with lower GABA levels were more vulnerable to developing PTSD after the incident [22].
Early traumatic experiences increase the risk of PTSD, and GABA deficits are involved in its development. An animal study found that juvenile traumatic stress-induced chronic anxiety and spatial memory loss and reduced expression of GABAA receptors, while exercise led to significant improvement [23].
6) High CRH
The corticotropin-releasing hormone (CRH) is produced by cells in the hypothalamus in response to physical or psychological stress, which consequently releases cortisol by the hypothalamic-pituitary-adrenal (HPA) axis.
A study on 61 war veterans showed increased CRH levels in PTSD patients compared to healthy controls [24].
Interestingly, PTSD patients tend to have high CRH, lower ACTH, and often low cortisol [25].
In animal studies, the activation of CRH receptors was involved in the initiation and post-trauma consolidation of stress effects on anxiety-like behavior, supporting the use of blockers for these receptors as potential prophylactic treatments for PTSD [26].
PTSD patients exhibited increased levels of CRH in a study on 11 war veterans, indicating the utility of compounds that dampen the CRH system in the treatment of PTSD [27].
7) Decreased Cannabinoids
Cannabinoid (CB) receptors (CB1 and CB2) play an important role in PTSD, specifically in stress responses [11].
CB1 receptors are found throughout the brain and control a variety of behaviors, including mood, stress, anxiety, learning, memory, and fear [11].
CB1 is found in a brain region responsible for fear that is implicated in PTSD. Genetic or pharmacological alterations of CB1 functions, which are required for normal fear extinction, result in anxiety for PTSD patients related to aversive memories [28, 29, 30].
PTSD may lead to increased alcoholism, and CB1 is sensitive to the effects of alcohol and traumatic stress. An animal study showed that PTSD blunts the behavioral sensitizing effects of alcohol in the brain. Also, mice exposed to stress and alcohol had decreased CB1 in the brain [31].
8) Increased Bodily Opioids
Opioids are the most widely used and effective painkillers for acute, strong pain. Opioid receptor activation following stress can not only increase pain relief, but also affect numerous behaviors including reward and depression [32].
Opioid receptors are located in brain regions that mediate anxiety-like behaviors and are implicated in the causes of PTSD [33].
Psychological Treatments
Several types of psychotherapy are used in people with PTSD. They can help you gain control of lasting fear and cope with stressful situations. You may discuss with your psychotherapist which approach or combination may be more convenient in your case. The treatment can consist of individual or group therapy, which offers the advantage of helping to connect with other people going through similar experiences.
1) Prolonged Exposure Therapy (PE)
PE is considered a gold standard protocol for the treatment of PTSD, which has shown effective in combat veterans [34].
2) Cognitive-behavioral therapy (CBT)
CBT helps patients to question and alter dysfunctional trauma-associated cognitions. In vivo or in sensu confrontation with trauma reminders helps patients to overcome their avoidance of situations and thoughts that are no longer dangerous, which leads to habituation and a reorganization of trauma memories finally [35].
3) Eye Movement Desensitization and Reprocessing (EMDR)
During EMDR, patients mentally focus on a trauma-associated disturbing image, memory, emotion, or cognition. In comparison to CBT, confrontation is rather short and interrupted by saccadic eye movements that are initiated by the therapist [35].
Drug Treatments
A wide range of medications have been studied for PTSD and a number are registered for this indication. Nevertheless, current treatments are only partially effective in some patients and are minimally effective in others. Potential new treatments need to and are being investigated, including glutamatergic, noradrenergic, and opioid pathways.
Work with your doctor to figure out what medication is most effective and causes the fewest adverse effects in your case. You may need to take one medication or a combination and adjust the dosage and medication schedule before finding the right fit for you. Remember to talk to your doctor if your symptoms don’t improve or you experience adverse effects.
Approved Drugs
Selective Serotonin Reuptake Inhibitors
Selective serotonin reuptake inhibitors (commonly known as SSRIs) allow for increased serotonin levels by preventing the clearing of serotonin from cellular receptors. Serotonin is an important brain molecule in the regulation of mood [36].
The SSRIs sertraline (Zoloft) and paroxetine (Paxil) are approved by the FDA for PTSD treatment.
In a clinical trial, 208 patients diagnosed with PTSD took either the selective serotonin reuptake inhibitor (sertraline) or a placebo. The patients given sertraline had a significant improvement in their symptoms (60%) over placebo (38%) [37].
However, selective serotonin reuptake inhibitors are not perfect. The drug takes weeks to show a therapeutic effect and has potential side effects, such as changes in appetite and loss of sexual drive [38].
The combinations of naltrexone and either the SSRI, paroxetine, or the NRI, desipramine, were studied in 88 veterans with PTSD and alcohol dependence. Desipramine had similar effects on PTSD symptoms as the standard SSRI treatment and was more effective in reducing alcohol consumption. Naltrexone reduced alcohol craving, without advantages on drinking use outcomes [39].
Off-Label Drugs
The following drugs are not approved by the FDA for PTSD treatment but some doctors may prescribe them (either alone or in combination with SSRIs and other drugs) in people who don’t respond to SSRIs alone.
1) Tricyclic Antidepressants
Tricyclic antidepressants (serotonin-noradrenaline reuptake inhibitors or SNRIs) inhibit the reuptake of the neurotransmitters serotonin and noradrenaline, controlling the biochemical pathways involved in anxiety. Two examples of tricyclic antidepressants are imipramine and amitriptyline [40, 41].
However, most tricyclic antidepressants, such as imipramine and amitriptyline, are not specific to a couple of receptors, which allows for many possible side effects. These side effects include blurred vision and constipation [40, 41].
Although SSRIs are the only FDA-approved medications for the treatment of PTSD, a study on 88 male veterans with PTSD suggested that SNRIs may have advantages over SSRIs [39].
2) Noradrenergic and Specific Serotonergic Antidepressants (NaSSA)
Mirtazapine is a noradrenergic and specific serotonergic antidepressant (NaSSA) that is approved in many countries for use in the treatment of depression. It is as effective as other antidepressants and may have a more rapid onset of action than selective serotonin reuptake inhibitors (SSRIs) [42].
Mirtazapine may also be effective in the treatment of anxiety disorders (including PTSD) [42].
In an 8-week pilot trial on 15 people with PTSD, mirtazapine improved PTSD symptoms and was well tolerated. Mirtazapine was also effective in the 12 patients who continued the study for 24 additional weeks [43, 44].
In another trial on 36 PTSD patients, the combination of mirtazapine and sertraline was more effective than the SSRI alone. In a trial on 51 war veterans comparing both drugs, mirtazapine was more effective and caused fewer adverse effects [45, 46].
3) Prazosin
Prazosin is a blocker of the alpha1-adrenergic receptors mainly used to treat high blood pressure and prostate enlargement.
Although the mechanism by which it does so remains unclear, prazosin seems to help with nightmares, insomnia, and psychological distress in people with PTSD, as seen in studies on almost 400 people [47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57].
However, there are some negative results as well. Prazosin only reduced alcohol consumption but not nighttime PTSD symptoms in a clinical trial on 30 people, and didn’t have any beneficial effects in 2 additional trials on 400 people [58, 59, 60].
4) Hydrocortisone
Animal studies have shown that treatment with hydrocortisone shortly after a traumatic event decreased the likelihood of suffering from PTSD [61].
In a clinical trial on 64 traumatic injury patients, a 10-day course of hydrocortisone improved PTSD and depression symptoms, and improved quality of life. People who had never received mental health treatments benefited the most from hydrocortisone [62].
5) Anti-Anxiety Medications
Anti-anxiety drugs can relieve severe anxiety in people with PTSD. Due to the potential for abuse of some drugs, they are generally used only for a short time.
The anti-anxiety drug buspirone reduced PTSD symptoms in 7 out of 8 patients in a small trial [63].
In contrast, benzodiazepines were ineffective at improving the symptoms and even worsened recovery in 3 clinical trials on almost 500 people with PTSD [64, 65, 66].
6) Ketamine
Ketamine is an anesthetic with psychoactive effects. It is a glutamate receptor blocker of the effects of excessive glutamate seen in most cases of PTSD [67].
In a study of 141 military burn victims, those who received ketamine had a PTSD prevalence of 26.9% while the prevalence reached 46.4% in the others [68].
However, due to the psychoactive nature of the drug, there could be a worsening of PTSD symptoms if the size and timing of dosages aren’t properly maintained [69].
In multiple studies of accident victims, ketamine increased symptoms of reexperiencing and dissociation. Given the mixed results from ketamine studies, other treatment options should be considered first [70, 71].
Complementary Strategies
Preliminary evidence suggests that the following complementary strategies may help as an add-on to your psychological and pharmacological treatment. You may discuss with your doctor if they may help in your case. Importantly, never implement these strategies in place of what your doctor recommends or prescribes.
1) Yoga
Yoga and other forms of meditation have a natural stress-relieving effect, which could help mitigate the hyperarousal symptoms of PTSD [72].
In a clinical trial on 49 young women with chronic PTSD, long-term yoga sessions greatly reduced PTSD symptoms and depression [73].
Multiple studies of people who underwent abusive or neglectful trauma found yoga to be effective at improving the depressive symptoms of the disease [74, 75].
Yoga can even help increase resilience from the disease, as a study of 12 military personnel, recently home from deployment showed decreased PTSD symptoms and increased mindfulness [76].
2) Cannabidiol
Cannabidiol (CBD) is a part of the cannabinoid family found in the marijuana plant Cannabis sativa, and, while similar to the compound THC (the active component in medical marijuana), cannabidiol does not produce psychoactive effects [77, 78].
The lack of psychoactive elements makes cannabidiol a prospective treatment for PTSD (given PTSD largely psychoactive symptoms). Other psychoactive drugs, such as ketamine, have a much more variable response to the disease [70].
CBD has been reported to reduce anxiety in 3 adults and 1 child with PTSD [79, 80].
In a study, rats given cannabidiol after experiencing and interacting with a predator (such as a cat). Repeated administration of cannabidiol after the interaction prevented long-term anxiety effects, which shows promise for PTSD treatment [81].
If your doctor determines that CBD may be helpful in your case, be sure to read through this post on the legal aspects of CBD worldwide to make sure you’re not breaking any laws.
3) Strenuous Exercise
Neuropeptide Y (NPY) is an important messaging molecule in the brain that helps suppress anxiety caused by increasing cortisol and corticotropin-releasing hormone (CRH), which are stress-response hormones [82].
The blood levels of NPY in soldiers undergoing extremely stressful prisoner of war exercises were higher after the exercises in a study on 49 soldiers. Those whose NPY level never returned to pre-exercise levels exhibited PTSD symptoms. These soldiers were found to have a depletion of NPY in their blood [83].
Strenuous exercise was found to increase NPY levels in a cell-based study, suggesting possible anti-anxiety benefits of exercise [84].
4) Sexual Activity
Animal studies showed that sexual activity counteracts the negative effects of chronic stress on the synthesis of new adult hippocampal neurons and recognition memory [85].