Red blood cells transport oxygen to all parts of the body. Read on to learn how nutrition affects red blood cell health, the optimal range for red blood cells, and the pros and cons of having high or lower levels of red blood cells.
Red Blood Cell Indices
Red blood cell indices are part of the complete blood count test. Each marker provides specific information about red blood cell health, which may be useful for diagnosing nutrient deficiencies and diseases.
Hemoglobin, hematocrit, and red blood cell indices are the initial laboratory tests used to diagnose and classify anemia.
Mean Corpuscular Volume (MCV)
Mean corpuscular volume (MCV) is a measurement of the average size (volume) of each red blood cell [1].
The normal values for MCV are 87 ± 7 fl (80 – 94 fl).
When red blood cells are smaller than normal (microcytic), the MCV is decreased. Low MCV is typical of a number of conditions, including:
- Copper deficiency [2]
- Iron deficiency [3]
- Vitamin C deficiency [4]
- Vitamin B6 deficiency [5]
- Vitamin A deficiency [6]
- Anemia of chronic disease [7]
- Thalassemia [8]
- Sideroblastic anemia [9]
- Rheumatoid arthritis [10]
- Lead toxicity [11]
When red blood cells are larger than normal (macrocytic), the MCV is increased. High MCV is typical of a number of conditions, including:
- Newborns and infants
- Megaloblastic anemias (folate deficiency anemia and vitamin B12 deficiency anemia) [12, 13]
- Reticulocytosis – increased red blood cell production (congenital hemolytic anemia and acute blood loss) [14]
- Alcoholism [15]
- Liver disease [16]
- Hypothyroidism [17]
- Aplastic anemia [16]
- Myelodysplastic syndrome [16]
- Acute leukemia [16]
- Drugs (methotrexate, antiretroviral, anticonvulsive, and sulfasalazine) [16]
These are not necessarily exhaustive lists of potential causes of high and low MCV, and they shouldn’t be used to self-diagnose anything. Your doctor will look at your MCV, other lab markers, and other symptoms to determine an appropriate diagnosis and treatment plan.
Mean Corpuscular Hemoglobin (MCH)
MCH quantifies the average amount of hemoglobin per red blood cell [1].
The normal values for MCH are 29 ± 2 picograms (pg) per cell (27-31 pg/cell).
Values of MCH typically mirror MCV results: small red blood cells have a lower MCH, and large red blood cells have a higher MCH. Thus, MCH is often increased and decreased in the same conditions as the MCV.
Mean Corpuscular Hemoglobin Concentration (MCHC)
MCHC indicates the amount of hemoglobin per unit volume of the red blood cell [1].
MCHC is the hemoglobin content divided by the volume of the red blood cell.
The normal values for MCHC are 34 ± 2 g/dl of red blood cells (32 – 36 g/dl).
Decreased MCHC values (hypochromia, or paler red blood cells) are seen in conditions such as iron deficiency anemia, vitamin B6 deficiency, and thalassemia [3, 8].
Increased MCHC values (hyperchromia, or darker color red blood cells) are seen in conditions such as autoimmune hemolytic anemia, in burn patients, and hereditary spherocytosis [18, 19].
Again, your doctor is best positioned to determine the underlying cause of irregular MCHC and to help you develop an appropriate treatment or management plan.
Red Cell Distribution Width (RDW)
RDW measures the variability of the red blood cell volume [1].
The normal value for RDW is 13 ± 1.5% (11.5 – 14.5%).
The RDW is often normal (homogenous red blood cell size) in healthy people and also in:
Doctors may therefore use RDW along with a battery of other tests to help them differentiate aplastic anemia from some other types of anemia.
High values (heterogenous red blood cells) indicate high variation in size (anisocytosis) of red blood cells. The RDW is often increased in:
- Vitamin B12 deficiency [12]
- Folate deficiency [21]
- Iron deficiency anemia [22, 23]
- Blood transfusions [24]
- Thalassemia [25]
- Sideroblastic anemia (abnormal red blood cells because the body cannot correctly incorporate iron into hemoglobin) [25]
- Alcoholism [26]
- Liver disease [27]
- Leukemia [28]
This is not necessarily an exhaustive list of potential causes of high RDW, and it shouldn’t be used to self-diagnose anything. Your doctor will look at your RDW, other lab markers, and other symptoms to determine an appropriate diagnosis and treatment plan.
No disease states have been identified in which the RDW is decreased [20].
RBC Count
RBC count is an estimate of the number of red blood cells per liter of the patient’s blood [29].
4.7 to 6.1 x 1012/L in adult men
4.2 to 5.4 x 1012/L in adult women
3.8 to 6.0 x 1012/L in children
Normal values may vary depending on the individual laboratory, the age of the patient, physical activity, and other factors [30].
If your RBC count is outside the normal range, talk to your doctor to determine the underlying cause and develop a management plan, if appropriate.
Red Blood Cell Production
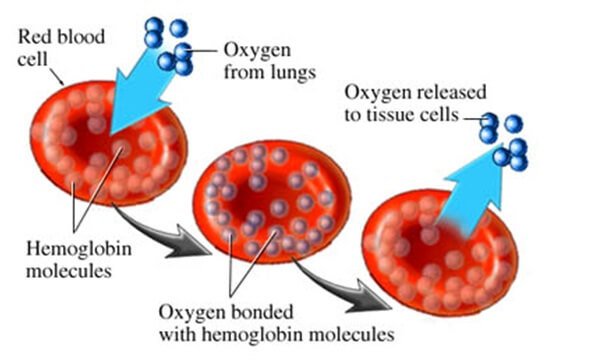
All blood cells originate from common parent cells called hematopoietic stem cells. In adults, blood cells are produced mainly in the bone marrow. Certain substances control the production of blood cells. The hormone erythropoietin or EPO, is produced in the kidneys and promotes the production of red blood cells [31].
The process by which red blood cells are produced is called erythropoiesis. This process relies on a number of nutrients and hormones to be efficient [32, 33]:
- Metals: iron, copper [34], zinc, manganese
- Vitamins: B12, folate, vitamins C, E, B6, thiamine (vitamin B1), riboflavin
- Amino acids
- Hormones: SCF (stem cell factor), IL-3, GM-SCF (granulocyte-macrophage stem cell factor), erythropoietin (EPO), androgens, and thyroxine.
How Are Red Blood Cells Disposed of in the Body?
Red blood cells have a life cycle of about 120 days. When they are too old or damaged, they are broken down in the bone marrow, spleen or liver.
Used up heme is broken down as a component of bile, which is excreted in the intestine [35].
What is Anemia?
Having a low level of red blood cells can diminish the ability of the blood to transport oxygen, which can cause the heart to come under strain as it works to get enough oxygen to the tissues [36].
Anemia can happen with lower red blood cell count or when red blood cells don’t contain enough hemoglobin [36].
In anemia, the body doesn’t get enough oxygen-rich blood. As a result, you may feel tired or weak. You also may have other symptoms, such as shortness of breath, dizziness, headaches, pale skin, chest pain, and coldness in the hands or feet [36, 37].
Severe or long-lasting anemia can damage your heart, brain, and other organs in your body. Very severe anemia may even cause death [36, 37].
What Causes Anemia?
Anemia is often a symptom that indicates another underlying condition. It’s important to talk to your doctor to identify the possible causes of your anemia and develop an appropriate treatment plan [36, 37].
The three main causes associated with anemia are:
- Blood loss
- Lack of red blood cell production
- Higher rates of red blood cell destruction
- Inflammation
For some people, the condition is caused by more than one of these factors [38]. Read this post on iron to learn more about anemia.
Inflammation and Anemia
The pro-inflammatory cytokines, IL-1, TNF-α, IFN-γ, and IL-6, inhibit red blood cell production in anemia [39].
IL-8 triggers the death (apoptosis) of red blood cells. RBCs are particularly sensitive to systemic inflammatory changes [40].
Symptoms of Anemia
Anemia is associated with a number of symptoms, which may indicate to your doctor that this test is appropriate. This is not necessarily an exhaustive list; someone with anemia count may have several of these symptoms in addition to others not listed here. Furthermore, these symptoms may not necessarily indicate anemia. Your doctor is best positioned to determine the appropriate blood tests, other labs, and treatment options.
That said, symptoms associated with anemia may include [41, 36, 37]:
- Headaches
- Dizziness
- Weakness
- Shortness of breath and problems breathing while lying down
- Double or blurred vision and blind spots
- Unexplained itching (especially after a warm bath), reddened face, and a burning feeling on your skin (especially your hands and feet)
- Bleeding from your gums and heavy bleeding from small cuts
- Unexplained weight loss
- Fatigue (feeling tired)
- Excessive sweating
- Coldness in the hands and feet
- Pale skin
- Chest pain
- Very painful swelling in a single joint, usually the big toe (called gouty arthritis)
- Bone pain (in rare cases)
- Increased probability of blood clots (impending danger of heart attack or stroke).
- Slowed blood flow also prevents enough oxygen-rich blood from reaching your organs. This can lead to angina (chest pain or discomfort) and heart failure. The high levels of red blood cells can lead to stomach ulcers, gout, or kidney stones.
- Some people may develop myelofibrosis. This is a condition in which your bone marrow is replaced with scar tissue. Abnormal bone marrow cells may begin to grow out of control which can lead to acute myelogenous leukemia (AML), a cancer of the blood and bone marrow. This disease can worsen very quickly [42].
- Arrhythmias or irregular heartbeats
- Heart damage and possibly heart failure
- Organ damage
- In people who have cancer or HIV/AIDS, anemia can worsen prognosis and reduce the effectiveness of treatments.
- People who have kidney disease with anemia are more likely to have heart problems [43]
Increased RBC count is independently (but weakly) associated with the risk of cardiovascular events [44].
Elderly patients with depression and low blood cell count may respond better to some medications such as fluoxetine [45].
Health Benefits of Having a Higher RBC Count
An increased number of red blood cells, to a certain extent, allows the body to transport more oxygen to muscles and therefore increase stamina and performance [46].
Conditions Associated With Low RBC Count
The conditions listed here are commonly associated with low RBC count but may indicate another condition or cause another set of symptoms. Work with your doctor or other health care professional for an accurate diagnosis.
1) Iron, Vitamin B6, B12, and/or Folic Acid deficiency
Approximately one-third of the world’s population is anemic, and the majority of these cases are due to iron deficiency [47].
A diet that lacks iron, folic acid, or vitamin B12 can prevent your body from making enough red blood cells. Your body also needs small amounts of vitamin C, riboflavin, and copper to make red blood cells [38].
Conditions that make it hard for your body to absorb nutrients also can prevent your body from making enough red blood cells [38].
Iron deficiency interferes with hemoglobin synthesis [48, 49], so iron deficiency results in reduced hemoglobin in red blood cells. Iron deficiency also results in more variable red blood cell size (>20% RDW), and smaller (low MCV) and paler red blood cells (low MCH) [48, 49].
Nutrient deficiency of either folate or vitamin B12 results in enlarged red blood cells (megaloblastic anemia), with an MCV increased to a range of 105 to 160 fl [49].
2) Inflammation and Infection
Some chronic diseases can cause anemia [37].
Anemia of inflammation is the second most common cause of anemia after iron deficiency. It is associated with acute and chronic infections, sepsis, malignancies, autoimmune disorders, and chronic kidney disease [39].
Some cancer treatments may damage the bone marrow or damage the red blood cells’ ability to carry oxygen. If the bone marrow is damaged, it can’t make red blood cells fast enough to replace the ones that die or are destroyed [37].
People who have HIV/AIDS may develop anemia due to secondary infections or medicines used to treat their diseases [37].
3) Pregnancy
Anemia can occur during pregnancy due to low levels of iron, folic acid, and/or vitamin B12 [37].
Anemia of pregnancy is considered a global health problem, affecting almost 50% of pregnant women [50].
During the first 6 months of pregnancy, the fluid portion of a woman’s blood increases faster than the number of red blood cells. This makes the blood thinner and can lead to anemia [37].
4) Smoking in Pregnancy
Smoking generally increases red blood cell count [51]. However, in pregnancy, smoking lowers red blood cell count which might create a hypoxic condition for the fetus [52].
Neonates born to smoking mothers had lower red blood cell counts, lower hemoglobin, and lower serum cobalamin levels [53].
5) Blood Loss
Blood loss is the most common cause of anemia, especially iron-deficiency anemia. Blood loss can be short term or persist over time.
Heavy menstrual periods or bleeding in the gut or urinary system can cause blood loss. Surgery, injury, or cancer also can cause blood loss [37].
6) Alcohol
Alcohol consumption decreases the red blood cell count, with even the lowest consumption producing a significant decrease in men [54]. In another study that showed similar results, there was a correlation between decreased RBCs and the duration of dependence [55].
7) Overhydration
Overhydration is rare, but can also occur in patients with impaired kidney function. The blood has more volume, but the number of blood cells is unchanged, resulting in a lower red blood cell count or concentration [56].
8) Low Erythropoietin
Your body needs the hormone erythropoietin to make red blood cells. This hormone is produced by the kidneys and stimulates the bone marrow to make more red blood cells [37].
Anemia is a common complication of chronic kidney diseases, due to reduced erythropoietin production by the kidneys [57, 58].
9) Enlarged or Diseased Spleen
The spleen is an organ that removes worn-out red blood cells from the body. If the spleen is enlarged or diseased, it may remove more red blood cells than normal, causing anemia [37].
10) Inherited and Acquired Conditions
Hereditary conditions such as sickle cell anemia or thalassemias can cause your body to destroy too many red blood cells, causing anemia [37].
Immune disorders, infections, certain medicines, or reactions to blood transfusions, can increase red blood cell destruction and cause hemolytic anemia [59].
Some infants are born without the ability to make enough red blood cells. This condition is called aplastic anemia. Infants and children who have aplastic anemia often need blood transfusions to increase the number of red blood cells in their blood [37].
Acquired conditions or factors, such as certain medicines, toxins, and infectious diseases, also can cause aplastic anemia [37].
11) Periodontal Disease
The progression of periodontal disease is associated with a decrease in red blood cell counts [60].
Chronic gum inflammation (periodontitis) is associated with a lower red blood cell count, which tends to improve after periodontal treatment [61].
Conditions Associated With High RBC Count
The conditions listed here are commonly associated with low RBC count but may indicate another condition or cause another set of symptoms. Work with your doctor or other health care professional for an accurate diagnosis.
High red blood cell count may be caused by low oxygen levels, kidney disease, or other problems.
1) Low Oxygen Levels or Hypoxia
Your body may increase red blood cell production to compensate for any condition that results in low oxygen levels, including:
- Living at high altitude [62]
- A condition present at birth that reduces the oxygen-carrying capacity of red blood cells (hemoglobinopathy) [63]
- Obstructive sleep apnea [64]
- Cystic fibrosis [65]
- Cor pulmonale [65]
- Congestive heart failure [65]
2) Obesity
Obesity has been linked with higher RBC count as well as a number of other elevated blood markers, though researchers are not sure why [66].
3) Bone Marrow Overproduction
- Polycythemia vera (when the bone marrow produces too many red blood cells) [67]
- Other myeloproliferative disorders (abnormal growth of blood cells in the bone marrow) [68]
4) Dehydration
If the liquid component of the blood is decreased, as in dehydration, the red blood cell count increases. Basically, the red blood cells become more concentrated, although their actual number stays the same [69].
5) Performance-Enhancing Drugs
Certain drugs stimulate the production of red blood cells, including:
6) Cold Exposure
Swimming in cold water can increase erythropoiesis (red blood cell production) [73].
In the elderly, red blood cell count was increased in the cold [74].
7) Smoking
Smoking increases red blood cell count except in pregnant women [51, 75, 76].



