Image credit: [1]
Somatostatin is known as the “boss” of the other hormones, but abnormal levels can cause health problems. Learn more about somatostatin.
What Is Somatostatin?
Somatostatin is a 14-amino acid peptide hormone that is in virtually every organ in the body. It acts as a hormone, a local regulator, and a neurotransmitter. Two scientists accidentally discovered it when they were dissecting the brain of a sheep.
Somatostatin is produced in the hypothalamus (the brain region that controls hormone secretion), the gut, and the pancreas (intestinal and pancreatic D cells) [2, 3, 4].
Somatostatin inhibits the release of hormones by binding to its five receptors (G-protein coupled receptors sst1 to sst5).
- sst2 and sst5 are located throughout the digestive tract, pancreas, and immune system. Most types of synthetic somatostatin bind to these two receptors.
- sst1, 2, 4, and 5 stop cell growth by activating proteins that suppress tumors and induce cell death (MAPK, tumor suppressor protein, and p21).
- sst3 triggers cell death by activating the proteins p53 and Bax.
A larger 28-amino acid hormone is the precursor to the 14-amino acid peptide. It binds more tightly to receptors and is 10 times stronger than normal somatostatin in inhibiting growth hormone and insulin secretion [5].
Because somatostatin influences most organs and tissues in the body, it is a hormone that rarely deviates from the normal range. When they do, they affect the production of other hormones: somatostatin excess reduces the levels of many other hormones, while its deficit has the opposite effect [6, 7].
Gut and Pancreatic Function
Somatostatin is released locally in the gut, concretely in hormone-secreting cells and nerve fibers, where it inhibits many hormones and reduces gut motility [8, 2, 9].
In the stomach, somatostatin inhibits stomach acid and stomach motility functions, slows down stomach emptying, and decreases the perception of fullness [2].
In the small bowel, somatostatin inhibits their function and blood flow, decreases fluid secretion, and increases absorption of water and electrolytes into the bloodstream. After a meal, somatostatin levels rise and inhibit glucose and fat absorption [8].
In the colon, somatostatin stimulates muscle contractions, increases transit time, and changes the function of the lining cells [2].
In the pancreas, somatostatin decreases the volume of this organ and inhibits the release of glucagon and insulin [2].
Somatostatin increases food consumption at low doses but has the opposite effect at higher doses. This hormone may also have pain-relieving effects and enhance learning [10].
Gut Hormone Regulation
Nutrients and high stomach acid levels (low pH) are the main stimulants of somatostatin release. Fats and proteins elicit a bigger somatostatin response than carbohydrates. Additionally, the following neurotransmitters, hormones, and drugs influence somatostatin release [2, 11]:
- The neurotransmitter acetylcholine stimulates somatostatin release after eating a meal.
- Gut peptides like gastrin, cholecystokinin, secretin, gastrin-releasing peptide, oxyntomodulin, and glucagon-like peptide also stimulate somatostatin.
- Substance P, insulin, pancreatic polypeptide, and opioids are potent inhibitors of somatostatin release.
Brain and Spinal Cord Function
Somatostatin-producing cells and receptors are widely distributed throughout several regions of the brain and spinal cord, including [10]:
- Hypothalamus: controls body temperature, thirst, hunger, hormone release by the pituitary gland, and, in part, sleep and emotions.
- Pituitary gland: secretes many hormones, including growth hormone, adrenocorticotropic hormone, and thyroid-stimulating hormone.
- Hippocampus: involved in memory and emotions.
- Cortex: plays an important role in memory, attention, and consciousness
- Brainstem: controls heart rate, breathing, sleeping, and eating.
- Spinal cord: sends messages to and from the brain to the rest of the body to control sensation and motor function.
Somatostatin has both inhibitory and excitatory effects on neurotransmitters and hormones [10]:
- Increases acetylcholine, serotonin, dopamine, norepinephrine, and epinephrine.
- Inhibits the release of growth hormone and thyroid-stimulating hormone.
Brain and Spinal Cord Regulation
Somatostatin is regulated by neurotransmitters and hormones in the brain [10]:
- Dopamine, acetylcholine, and growth hormone increase somatostatin, while GABA and adrenocorticotropic hormone inhibit it.
- Neurotensin stimulates somatostatin secretion in the hypothalamus and part of the cortex (neocortex).
- Vasoactive intestinal peptide inhibits somatostatin secretion in the hypothalamus but stimulates its release from the neocortex.
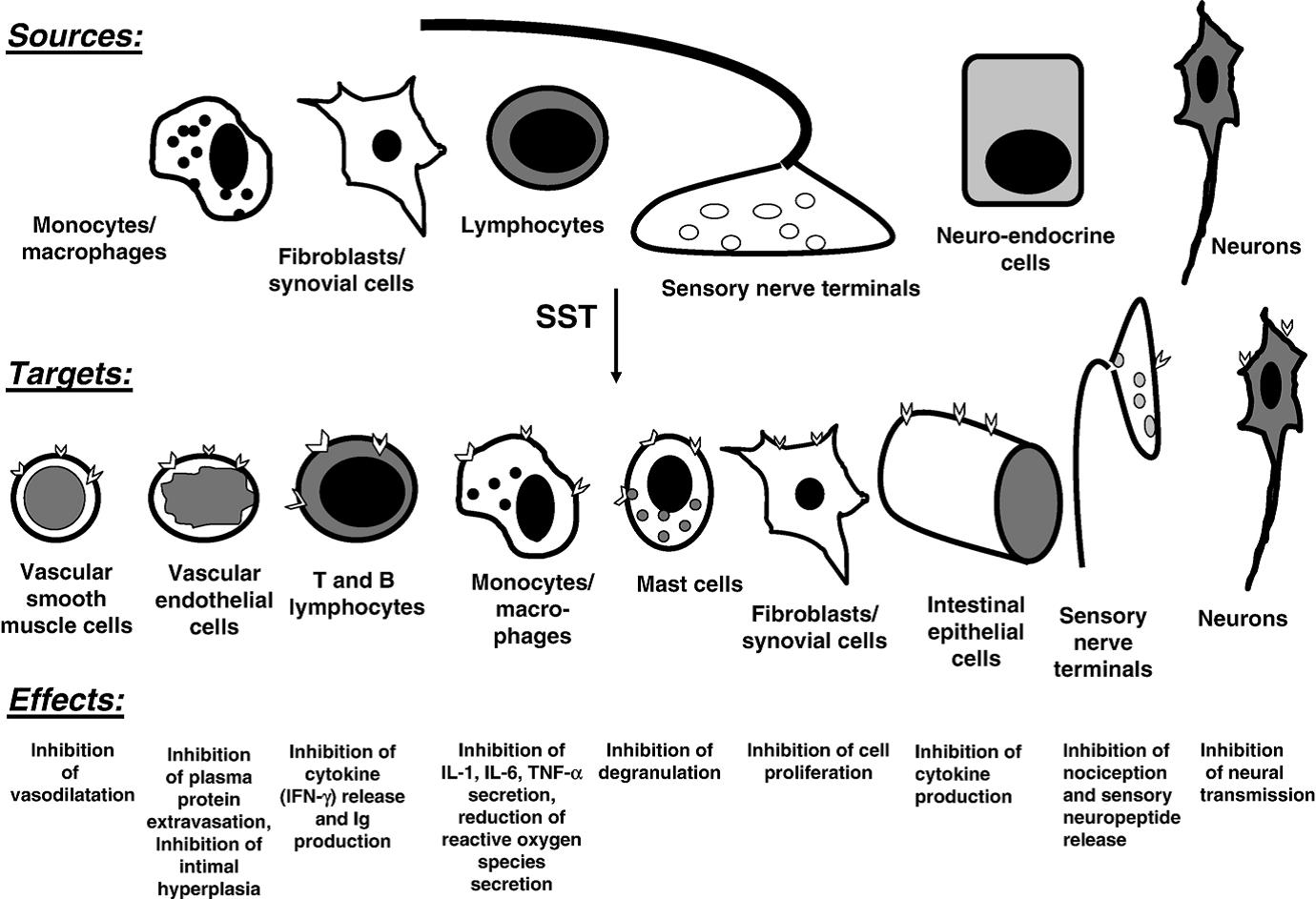
Immune Function
Somatostatin allows the nervous, hormone, and immune system to communicate with one another. This hormone has a number of effects on the immune function [12, 13]:
- Both suppress and stimulates the reproduction of immune cells (lymphocytes).
- Inhibits the function of other white blood cells (natural killer cells and monocytes).
- Reduces antibiotic production.
- Lowers the release of inflammatory cytokines (IFN-g).
Somatostatin receptors are present in white blood cells and the following organs of the immune system [13]:
- Lymph nodes
- Tonsils
- Spleen
- Thymus
Both injection and local treatment with somatostatin have the potential to help with autoimmune diseases and chronic inflammation [12].
Sleep Function
In a clinical trial on 7 elderly people, somatostatin disrupted sleep quality by decreasing total sleep and dream (REM) time. Somatostatin has also been reported to decrease deep sleep (slow wave sleep), during which growth hormone is released and immune function is repaired [14, 10].
Bone Function
Somatostatin may inhibit bone growth by locally reducing the reproduction and growth of cartilage and bone precursor cells [15].
When injected with insulin, somatostatin has the potential to reduce the calcified cartilage and brittle bones caused by diabetes, as seen in a rat study. Somatostatin reduced bone and cartilage growth and development by inhibiting insulin-dependent cell production. It also reduced blood vessel invasion that leads to weak joints and brittle bones [16].
Health Benefits
Although somatostatin is not often used in medicine, synthetic somatostatin can treat various diseases. Somatostatin analogs have similar molecular structures and mimic its effects. While somatostatin binds to all five somatostatin receptors, the analogs only bind to specific receptors [2].
Commonly used somatostatin analogs include:
- Octreotide: binds primarily to sst2 and helps control hormone over-secretion in patients with hormone-producing tumors [17, 18].
- Pasireotide: binds tightly to sst5 and is used to treat Cushing’s disease and acromegaly [19].
- Lanreotide: binds tightly to sst2 and less so to sst5. It is used to treat acromegaly and tumors in the stomach, intestines, and pancreas [17].
Effective for:
1) Hormone-Producing Tumors
Tumors that produce hormones occur most often in the digestive tract, pancreas, or lungs. Hormone-producing tumors are hard to diagnose due to their non-specific and variable symptoms. More than 50% of these tumors cannot be surgically removed after diagnosis [20].
Somatostatin analogs can treat symptoms caused by the overproduction of hormones from these tumors. Octreotide can prevent low blood potassium levels, dehydration, and diarrhea in cancer patients with hormone-producing tumors [2].
In a clinical trial on 41 people with hormone-producing tumors in the gut and lungs, injected octreotide led to a 24% response rate and a 2-year survival rate of around 76%. Octreotide is an effective treatment for patients with therapy-resistant and progressive cancer [21, 20].
Several meta-analyses attest to the effectiveness of somatostatin analogs against carcinoid tumors of the pancreas and gastrointestinal tract [22, 23, 20].
Somatostatin analogs may also help treat non-hormone-producing tumors. Somatostatin stops tumor growth by inhibiting the release of the hormones that stimulate their growth and preventing the formation of new blood vessels [24].
For instance, meta-analyses found them effective against the following hormone-responsive cancer types:
- Breast cancer [25]
- Liver cancer (in Asian populations) [26]
- Meningeal tumors [27]
- Prostate cancer [28]
2) Acromegaly
Excess growth hormone production due to tumors in the pituitary gland causes acromegaly. Symptoms include enlargement of the face, hands, and feet. Somatostatin analogs are used when surgery is ineffective in controlling the disease [29].
In a clinical trial on over 350 people with acromegaly, the analogs pasireotide and octreotide significantly reduced tumor size [30].
Somatostatin stops tumor cell growth by activating pathways that prevent cells from dividing (p21 and p27). Somatostatin also reduces symptoms associated with the disease, like heart, sleep, and insulin dysfunction [31, 29].
The main conclusions from the different meta-analyses on somatostatin analog therapy for acromegaly are:
- Long-acting release octreotide shrinks tumors in over 50% of patients with acromegaly. It is more effective than slow-release lanreotide [32, 33].
- Pretreatment with somatostatin analogs improves acromegaly control 3 months after surgery [34].
- Somatostatin analogs have reduced the death rate in people with acromegaly [35].
3) Cushing’s Disease
Cushing’s syndrome is a condition caused by excessive exposure to glucocorticoids such as cortisol. Its symptoms include obesity, thin skin, short stature, high blood pressure, anxiety, depression, bruising, glucose intolerance, and weakness [36].
When the disease is caused by pituitary tumors that produce adrenocorticotropic hormone (ACTH), it’s called Cushing’s disease. High levels of ACTH lead to high levels of cortisol, which can damage many tissues and organs in the body [31, 37].
The main treatments for these conditions are reducing or discontinuing corticosteroid medication (in people with Cushing’s syndrome due to long-term corticosteroid use) or the surgical removal of the tumor (in people with Cushing’s disease). Radiation therapy may be prescribed if the tumor cannot be completely removed with surgery [38].
If the surgery is unsuccessful or cannot be carried out, the doctor may prescribe pasireotide injections (2x/day). Pasireotide targets pituitary tumors and reduces cortisol levels, which lowers body weight, blood pressure, and cholesterol levels [31, 37].
Although pasireotide is effective in treating Cushing’s disease, it can cause high blood sugar levels by inhibiting 2 hormones (glucagon-like peptide-1 and glucose-dependent insulinotropic polypeptide). In people with type 2 diabetes or glucose intolerance, mifepristone can block the effects of cortisol in the tissues without affecting blood sugar levels [37].
In a clinical trial on 38 people with ACTH-independent Cushing’s syndrome, octreotide temporarily suppressed cortisol secretion. However, it was not effective for other forms of this syndrome [39].
Possibly Effective
1) Polycystic Kidney and Liver Disease
In 3 clinical trials on 153 people with polycystic kidney disease, octreotide slowed kidney growth, thus reducing cyst volume by 50%. Octreotide was safe, well-tolerated, and also reduced blood pressure and body weight [40, 41, 42].
However, lanreotide was ineffective at reducing the decline of kidney function and increased the risk of infected cysts in a clinical trial on over 300 people [43, 44].
This drug was, however, effective at reducing liver growth in clinical trials on 238 people with polycystic liver disease followed up for up to 18 months. Nevertheless, a continuous treatment was needed to maintain the effects and the drug had no effect on weight and muscle loss [45, 46, 47, 48].
Ocreotide had similar effects in clinical trials on 56 people with polycystic liver disease. Its effects were not enhanced by adding the immunosuppressant everolimus [49, 50].
In a clinical trial on 42 people with severe polycystic liver disease resulting from polycystic kidney or liver disease followed up for 2 years, octreotide was safe and slowed down the progressive increase in liver and kidney volume. This drug was also effective in a trial on 27 people with simultaneous polycystic kidney and liver disease [51, 52, 53].
All in all, the evidence supports this potential use of somatostatin. You may discuss with your doctor if somatostatin may be effective as an add-on to your treatment regime. Never use somatostatin in place of what your doctor recommends or prescribes.
2) Pancreatitis
Pancreatitis is a severe inflammation of the pancreas. Acute pancreatitis is caused by digestive enzymes damaging pancreatic tissue, often as a complication of an endoscopy, whereas chronic pancreatitis is pancreatic failure commonly resulting from alcoholism [54].
Somatostatin and octreotide reduced the death rate for acute pancreatitis and relieved pain for chronic pancreatitis in several clinical trials. Octreotide may reduce inflammation in the pancreas by inhibiting cells and pathways (intestinal mucosal mast cells and TLR4–NF-kB cytokine pathway) that produce an inflammatory immune response [54, 55].
Several meta-analyses on the use of somatostatin and octreotide to prevent acute pancreatitis found them effective, especially when given as a single bolus or a long-term infusion, or at high doses [56, 57, 58, 59, 60]
However, octreotide did not stop progression or reduce pain in a clinical trial on 302 people with chronic pancreatitis. The use of somatostatin analogs to treat chronic pancreatitis is controversial and scientific studies yield mixed results [61].
Taken together, the evidence suggests that somatostatin and its analogs may help with acute pancreatitis. Your doctor may determine if it can help in your case.
3) Ulcers
Somatostatin helped treat stomach ulcer bleeding in a clinical trial on 43 people by reducing stomach acid secretion and blood flow to the stomach. Both somatostatin and its analog octreotide were similarly effective in a few other trials, most of them from the 80s [62, 63, 64, 65, 66].
A meta-analysis concluded that somatostatin may help as an add-on before an endoscopy or when this procedure cannot be conducted successfully [67].
A study on 28 people associated low somatostatin levels with intestinal ulcers. In these patients, the somatostatin suppression inhibited stomach acid function, which was restored after treating the ulcers [68].
Although the evidence is limited and most studies are old, somatostatin seems to help with stomach ulcers. However, approved treatments such as histamine blockers or proton pump inhibitors may be more effective. You may discuss the possibility to use somatostatin as an add-on to your medication.
Insufficient Evidence
1) Fistulas
Fistulas are abnormal connections between blood vessels, intestines, or other hollow organs. Gut fistulas are the most common cause of severe intestinal failure [69].
In a clinical trial on 40 post-surgical patients, direct infusion of somatostatin into gastrointestinal fistulas and nutrients into the gut significantly decreased fistula closure time. Somatostatin inhibited the effect of gut hormones and decreased gut muscle contractions, while nutrient infusion prevented nutrient imbalance [70].
Somatostatin and its analogs also decreased fistula closure time in another trial on 33 people, although the results were not statistically significant [69].
Somatostatin also reduced the incidence of post-surgical pancreatic fistulas by reducing secretions by this organ in a clinical trial on 67 people [71].
Both somatostatin and octreotide were similarly effective at preventing post-surgical pancreatic fistulas in 2 trials on 71 people. However, octreotide was ineffective in two trials on over 400 people [72, 73, 74, 75].
Lanreotide improved pancreatic and gastrointestinal fistulas in 35 out of 54 patients (almost 65%) in a clinical trial [76].
Pasireotide also reduced the incidence of pancreatic fistulas after surgery in a clinical trial on 300 people, thus reducing the cost of the procedure [77, 78].
However, the most recent meta-analysis concluded that somatostatin and its analogs had modest effects on fistula prevention (e.g., reducing closure time but not closing rate or mortality) or found insufficient evidence of their effectiveness [79, 80, 81, 82, 83, 84, 85, 86].
Despite the abundance of trials, the results are inconclusive. Larger, more robust clinical trials are needed to shed some light on the potential benefits of somatostatin in people at risk of developing fistulas.
2) Diabetes
Somatostatin is produced in the pancreas (islet D cells) and locally inhibits insulin and glucagon. Insulin reduces blood sugar levels, while glucagon increases them [5].
Somatostatin and insulin helped control excess blood sugar more effectively than insulin alone in a small trial on 10 diabetic patients [87].
Somatostatin inhibits glucagon and growth hormone, which prevents an increase in blood sugar. It also reduces high blood sugar after consuming food by inhibiting carbohydrate absorption in the digestive tract [87, 5, 88].
Even if it may help with blood sugar control, the effects of somatostatin only last for half an hour, which makes it less effective than insulin and antidiabetic medication [5].
More recently, diabetes has been associated with a reduced production of glucagon in response to low blood sugar, an effect that can be corrected with somatostatin blockers. For this reason, these agents have been suggested as an add-on to insulin therapy to prevent blood sugar levels to drop too low [38].
Taken together, the evidence is mixed and doesn’t allow us to draw conclusions on whether somatostatin improves or worsens diabetes. More clinical research is needed to clarify this subject.
3) Arthritis
Somatostatin injection into the joints reduced pain at rest and on movement, joint tenderness, morning stiffness, spontaneous pain, and synovial thickness in 2 small trials on 57 people with rheumatoid arthritis. This treatment also reduced pain and improved joint function in another trial on 20 people with knee osteoarthritis [89, 90, 91].
In a more recent pilot study on 10 people with rheumatoid arthritis, intramuscular injections of octreotide for three months reduced pain and the number of swollen joints in weeks 8 to 10 but had less effect by week 12 [92].
The combination of somatostatin and gold salts improved psoriatic arthritis in another trial on 60 people [93].
A study associated rheumatoid arthritis with an increased ratio of growth hormone over somatostatin [94].
Octreotide and pasireotide reduced joint swelling and pain in a mouse model of arthritis by binding to sst2 [95].
Although the results are promising, a few small clinical trials and a study in mice cannot be considered sufficient evidence to claim that somatostatin improves arthritis. More clinical trials on larger populations are needed to confirm these preliminary findings.
4) Diarrhea
People with Irritable bowel syndrome (IBS) have overly sensitive intestines. Octreotide reduced discomfort and the feeling of fullness in the large intestines in a small trial on 8 people with diarrhea-prone IBS [96].
A gel with lanreotide improved the symptoms in a clinical trial on 33 people with chronic diarrhea of unknown cause [97].
Somatostatin analogs may prevent diarrhea by slowing gut transit time, decreasing abnormal fluid secretion into the intestines, and increasing the absorption of water and electrolytes into the bloodstream. Octreotide may also increase the threshold for intestinal discomfort by inhibiting the release of serotonin from stomach glands [98, 2].
Two clinical trials are clearly insufficient to support this potential use of somatostatin. Further clinical research is needed to validate their results.
5) Obesity
In a clinical trial on 39 healthy people, octreotide slowed stomach emptying and increased stomach volume, but also decreased the feelings of fullness after eating a meal [99].
In a clinical trial on 18 children with hypothalamic obesity, octreotide suppressed insulin secretion, which stabilized their weight and body mass index [100].
Again, only two small clinical trials support this health benefit. We cannot claim for certain that somatostatin helps with obesity until more research is conducted.
Side Effects
This list does not cover all possible side effects. Contact your doctor or pharmacist if you notice any other side effects.
Call your doctor for medical advice about side effects. In the US, you may report side effects to the FDA at 1-800-FDA-1088 or at www.fda.gov/medwatch. In Canada, you may report side effects to Health Canada at 1-866-234-2345.
Common side effects observed in clinical trials include [29, 101]:
- Stomach discomfort
- Loss of appetite
- Diarrhea
- Gas
- Nausea
- Vomiting
- Pain
- Fatigue
- Headache
- Dizziness
- Excess fat in the stools
- Gallstones
Some analogs like pasireotide and octreotide can cause high blood sugar. Long-term use of octreotide can also result in growth hormone deficiency, which may cause [37, 102]:
- Changes in body composition, such as excessive body fat and muscle wasting
- Decreased muscle strength and exercise capacity
- Increased risk of heart disease
- Reduced psychological well-being and quality of life
Diseases Linked to High Levels of Somatostatin
The following conditions are commonly associated with high somatostatin levels, but this single symptom is not enough for a diagnosis. Work with your doctor to discover what underlying condition might be causing your unusually high levels of this hormone and to develop an appropriate plan to improve your health:
- Somatostatin-producing tumors (Somatostatinomas) [103, 104]
- Brain and Spinal Cord tumors [105, 10]
- Huntington’s Disease [106, 107, 108]
- Spinal Cord Disease [105, 10]
- Intervertebral Disc Disease [105, 10]
- Post-Traumatic Stress Disorder [109]
- Anorexia [110]
- Irritable Bowel Syndrome [111]
- Gallstones [112]
Diseases Linked to Low Levels of Somatostatin
The following conditions are commonly associated with low somatostatin levels, but this single symptom is not enough for a diagnosis. Work with your doctor to discover what underlying condition might be causing your unusually low levels of this hormone and to develop an appropriate plan to improve your health:

